Hepatitis C is a serious viral infection that affects the liver, leading to inflammation and potential long-term complications if left untreated. The Hepatitis C virus (HCV) primarily spreads through blood-to-blood contact and can lead to both acute and chronic infections. Globally, millions of people are living with the infection, many without realizing it because symptoms often appear only in advanced stages.
Early detection and treatment can prevent liver damage and significantly improve outcomes.
What is Hepatitis C?
It is an infectious disease caused by the Hepatitis C virus that primarily attacks liver cells. Over time, this infection can cause inflammation, fibrosis (scarring), cirrhosis (severe liver damage), or even liver cancer.
Unlike Hepatitis A and B, there is no vaccine for Hepatitis C. However, with the advancement of antiviral therapies, the condition is now curable in most cases with timely medical intervention.
How is Hepatitis C Transmitted?
Hepatitis C spreads when infected blood enters another person’s bloodstream. Common transmission routes include:
Unsafe medical practices such as using unsterilized needles or equipment.
Sharing needles among intravenous drug users.
Blood transfusions received before the introduction of routine screening (before 1992 in many countries).
Tattooing or body piercing with contaminated instruments.
Mother-to-child transmission during childbirth (rare).
Unprotected sexual contact, particularly among individuals with multiple partners or sexually transmitted infections.
It’s important to note that Hepatitis C is not spread through casual contact such as hugging, kissing, or sharing utensils.
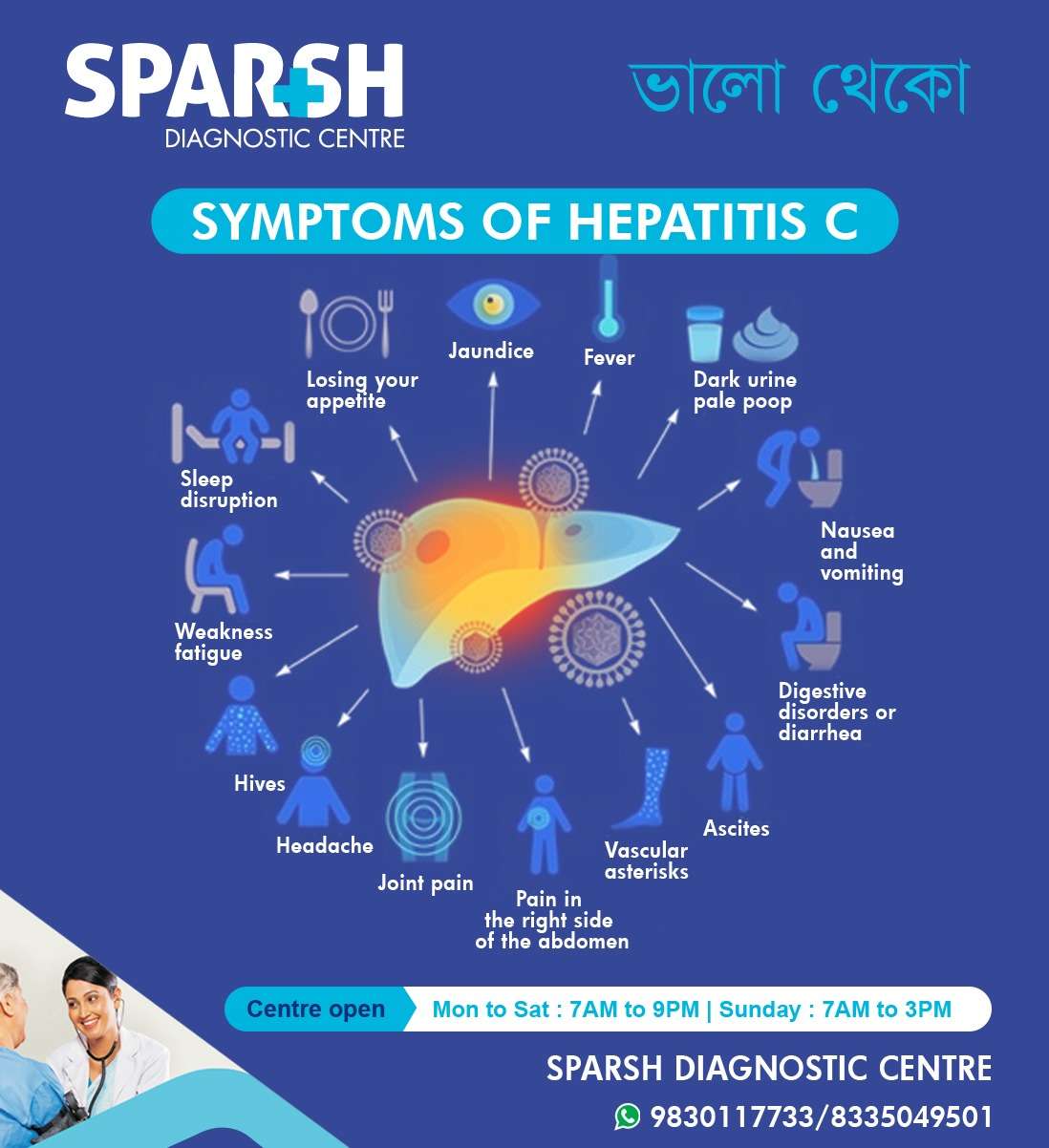
Symptoms of Hepatitis C
Many people with Hepatitis C do not experience symptoms for years. However, when symptoms appear, they can include:
Jaundice – Yellowing of the skin and eyes due to increased bilirubin.
Fever – Mild to moderate fever indicating infection.
Dark urine and pale stool – A sign of impaired liver function.
Nausea and vomiting – Common digestive symptoms.
Loss of appetite – Leading to unintentional weight loss.
Fatigue and weakness – Persistent tiredness due to liver stress.
Headache and joint pain – Due to systemic inflammation.
Abdominal pain – Especially on the right side, where the liver is located.
Digestive disorders or diarrhea.
Sleep disturbances and brain fog.
Hives and skin rashes.
Ascites (fluid accumulation in the abdomen) – Often seen in chronic cases.
Vascular asterisks (spider-like blood vessels) – Visible on the skin in advanced stages.
If you notice any of these symptoms, it’s crucial to get tested promptly. Sparsh Diagnostic Centre offers liver function tests, antibody screening, and HCV RNA tests for early diagnosis.
Stages of Hepatitis C
Hepatitis C infection progresses through several stages:
1. Acute Hepatitis C
Develops within six months after exposure to the virus.
About 15–25% of patients clear the virus naturally without treatment.
The rest develop chronic Hepatitis C.
2. Chronic Hepatitis C
The virus persists in the body for more than six months.
Chronic infection can last for decades and damage the liver gradually.
3. Cirrhosis
Long-term liver inflammation leads to scarring and loss of liver function.
Cirrhosis increases the risk of liver failure and liver cancer.
4. Liver Cancer (Hepatocellular Carcinoma)
Untreated chronic Hepatitis C can eventually lead to liver cancer.
Regular monitoring is crucial for those with cirrhosis or chronic infection.
Diagnosis of Hepatitis C
Accurate diagnosis is essential for managing Hepatitis C. At Sparsh Diagnostic Centre, we use advanced diagnostic tests to detect and evaluate the infection, such as:
Anti-HCV Antibody Test – Detects antibodies that the body produces against the Hepatitis C virus.
HCV RNA Test (PCR Test) – Confirms active infection by detecting viral RNA in the blood.
Liver Function Test (LFT) – Assesses liver enzyme levels to gauge liver health.
Fibroscan or Ultrasound – Measures liver stiffness to detect fibrosis or cirrhosis.
Genotype Testing – Determines the strain of the virus to tailor treatment.
Getting tested early allows for timely treatment and prevents serious liver complications.
Treatment Options for Hepatitis C
Hepatitis C is now considered a curable disease in most patients. The main goal of treatment is to eliminate the virus and prevent liver damage.
1. Antiviral Medications
Direct-Acting Antivirals (DAAs): These are the most effective medications, curing over 95% of patients with minimal side effects.
Common DAAs include Sofosbuvir, Ledipasvir, Velpatasvir, and Glecaprevir.
Treatment usually lasts for 8 to 12 weeks.
2. Supportive Care
Avoid alcohol and smoking, as these worsen liver damage.
Maintain a balanced diet rich in fruits, vegetables, and lean proteins.
Get vaccinated for Hepatitis A and B to prevent co-infection.
Regular monitoring of liver function is essential.
3. Liver Transplant
In advanced stages (cirrhosis or liver failure), a liver transplant may be required. Antiviral therapy is often continued before and after transplant to prevent reinfection.
Prevention of Hepatitis C
Although no vaccine exists, you can take preventive steps to reduce the risk of infection:
Never share needles, razors, or toothbrushes.
Ensure sterile conditions during tattoos, piercings, or medical procedures.
Use condoms during sexual contact with new or multiple partners.
Donate or receive blood only from licensed centers.
Get tested regularly if you’re in a high-risk group (e.g., healthcare workers, dialysis patients, or people with a history of blood transfusions).
Complications of Hepatitis C
If left untreated, Hepatitis C can lead to severe and life-threatening complications:
Chronic liver disease
Lifestyle Tips for Hepatitis C Patients
Eat a liver-friendly diet – Include plenty of fruits, vegetables, and whole grains.
Stay hydrated – Drink enough water to support liver detoxification.
Exercise regularly – Helps reduce fatigue and maintain overall health.
Avoid alcohol – Alcohol accelerates liver damage.
Take medicines only as prescribed – Some drugs can stress the liver.
Get regular checkups – Monitor liver function and viral load periodically.
Hepatitis C and Pregnancy
Pregnant women infected with Hepatitis C can transmit the virus to their newborns, though the risk is relatively low (about 5–6%). Routine prenatal screening is essential. Modern antiviral treatments are generally postponed until after childbirth due to limited safety data during pregnancy.
Why Choose Sparsh Diagnostic Centre for Hepatitis C Testing?
At Sparsh Diagnostic Centre, we prioritize your liver health through:
Accurate HCV testing using advanced laboratory techniques.
Comprehensive liver function assessments.
Expert consultation and guidance for managing liver conditions.
Quick turnaround time for reports.
Compassionate care and patient education to ensure long-term wellness.
We are committed to early detection and effective management of Hepatitis C to help you lead a healthier life.
Frequently Asked Questions (FAQs)
1. What causes Hepatitis C?
It is caused by the Hepatitis C virus (HCV), which spreads through contact with infected blood.
2. Can it be cured?
Yes. With modern antiviral medications, Hepatitis C can be completely cured in more than 95% of patients.
3. How long does treatment take?
Most antiviral regimens last between 8 to 12 weeks, depending on the viral genotype and liver condition.
4. What foods should I avoid with Hepatitis C?
Avoid alcohol, processed foods, fried items, and foods high in saturated fats. Instead, focus on fresh fruits, vegetables, and whole grains.
5. Can it return after cure?
Once cured, the same virus cannot return. However, you can get reinfected if exposed again to the virus.
6. Is it contagious?
Yes, but it spreads only through blood contact—not casual touch, sharing food, or kissing.
7. Can I prevent Hepatitis C?
Yes. Avoid sharing needles, ensure safe medical practices, and get tested regularly if you are at risk.
8. When should I get tested?
If you use injectable drugs, or have unexplained liver issues, you should get tested immediately.
To get tested and treated for Hepatitis C at Sparsh Diagnostic Centre, call our helpline number 9830117733.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()






[…] Hepatitis C […]
[…] a viral infection, it is known as hepatitis. Among the different types of viral hepatitis — A, B, C, D, and E — Hepatitis E is a lesser-known yet significant public health concern, especially in […]
[…] Caput Medusae. Long-term liver damage from conditions like alcoholic liver disease, hepatitis B or C, or non-alcoholic fatty liver disease (NAFLD) leads to scar tissue formation. This fibrosis […]
[…] Hepatitis infections (B, C) […]
[…] B, hepatitis C, HIV, and malaria can trigger nephrotic […]
[…] (A, B, C, etc.): Viral infections can inflame the […]
[…] Hepatitis C […]
[…] Hepatitis C […]
[…] hepatitis B and C […]
[…] B and C: These viral infections are linked to glomerular […]
[…] Viral infections (hepatitis A, B, C), alcohol abuse, autoimmune reactions, or […]
[…] B and C: Chronic infection with these viruses can lead to liver cirrhosis, which increases the risk of […]
[…] infections (Hepatitis B, Hepatitis C, […]
[…] Hepatitis B or Hepatitis C virus infections are major contributors to cirrhosis. These infections can lead to inflammation and […]