Cholangitis is a potentially life-threatening condition involving inflammation of the bile ducts. These ducts are essential for transporting bile — a fluid that aids in the digestion of fats — from the liver and gallbladder to the small intestine. When these ducts become blocked or infected, it can lead to a medical emergency requiring prompt diagnosis and treatment.
This blog from Sparsh Diagnostic Centre offers a complete overview of cholangitis, including its symptoms, causes, diagnostic tests, complications, and treatment options.
What is Cholangitis?
Cholangitis is the inflammation of the bile ducts, usually due to an obstruction followed by bacterial infection. The most common form is acute ascending cholangitis, where bacteria ascend from the duodenum into the biliary tree. This condition can progress rapidly and cause sepsis or liver damage if not treated urgently.
Types of Cholangitis
There are several types of cholangitis, each with different causes and clinical presentations:
1. Acute (Ascending) Cholangitis
This is the most common and serious form. It usually results from a bile duct obstruction, often due to gallstones, strictures, or tumors.
2. Primary Sclerosing Cholangitis (PSC)
An autoimmune condition causing chronic inflammation and scarring of the bile ducts, often associated with inflammatory bowel disease (IBD), especially ulcerative colitis.
3. Secondary Sclerosing Cholangitis
Occurs due to known causes like infections, surgery, trauma, or ischemia affecting the bile ducts.
4. Recurrent Pyogenic Cholangitis
Common in Southeast Asia, this chronic condition is caused by repeated bacterial infections and intrahepatic pigment stones.
Symptoms of Cholangitis
Symptoms can vary based on the severity and type of cholangitis. The classic presentation is known as Charcot’s Triad:
If left untreated, it may progress to Reynolds’ Pentad, which includes the above triad plus:
Altered mental status
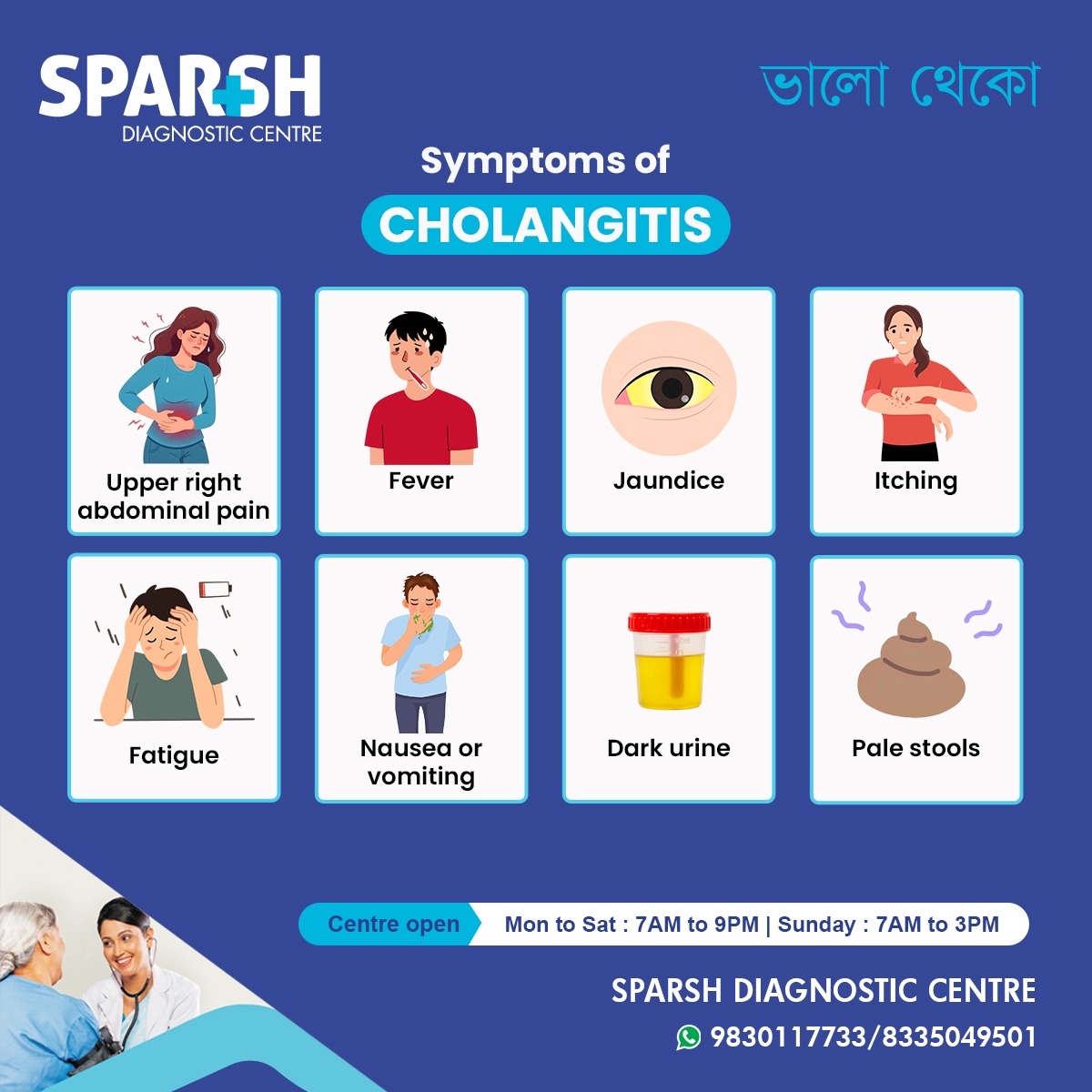
According to the visual infographic by Sparsh Diagnostic Centre, common symptoms include:
Upper Right Abdominal Pain – Persistent or sharp pain under the right ribcage.
Fever – Often with chills, indicating infection.
Jaundice – Yellowing of the skin and eyes due to bile backup.
Itching – Due to bile salts accumulating under the skin.
Fatigue – Caused by systemic inflammation and liver dysfunction.
Nausea or Vomiting – Often due to bile duct obstruction.
Dark Urine – A result of excess bilirubin excretion.
Pale Stools – Indicating a lack of bile in the digestive tract.
Causes of Cholangitis
Cholangitis usually occurs when there is a blockage or infection in the bile ducts. Common causes include:
1. Gallstones (Choledocholithiasis)
The most common cause of acute cholangitis. Stones can migrate from the gallbladder and obstruct the common bile duct.
2. Bile Duct Strictures
These are narrowings of the bile ducts that may result from:
Surgery
Primary sclerosing cholangitis
3. Bile Duct Tumors
Cancerous or benign growths can block bile flow, leading to inflammation and infection.
4. Parasites
Liver flukes or roundworms can obstruct bile ducts in endemic areas.
5. Medical Procedures
Endoscopic retrograde cholangiopancreatography (ERCP) or liver transplantation can occasionally introduce bacteria into the bile ducts.
Who is at Risk?
People with the following risk factors are more likely to develop cholangitis:
Gallstones
History of bile duct surgery
Previous ERCP
Primary sclerosing cholangitis
Pancreatic or biliary cancers
Living in or traveling to regions endemic for liver flukes
Diagnosis of Cholangitis
Diagnosing cholangitis involves clinical evaluation, imaging tests, and laboratory investigations.
1. Medical History & Physical Exam
The doctor will assess the presence of Charcot’s Triad and look for signs of sepsis or liver failure.
2. Blood Tests
CBC: Elevated white blood cells
Liver Function Tests (LFTs): Elevated bilirubin, ALP, ALT, and AST
Procalcitonin/CRP: To assess infection and inflammation
Blood cultures: To identify bacterial organisms
3. Imaging Tests
Ultrasound: First-line tool to detect bile duct dilatation or stones
CT Scan: Useful for assessing complications
MRCP (Magnetic Resonance Cholangiopancreatography): Non-invasive imaging of bile ducts
ERCP (Endoscopic Retrograde Cholangiopancreatography): Both diagnostic and therapeutic
Treatment of Cholangitis
Cholangitis is a medical emergency that requires prompt treatment.
1. Hospitalization
Most patients with acute cholangitis need to be admitted for close monitoring and intravenous therapy.
2. Antibiotics
Broad-spectrum IV antibiotics are initiated to combat gram-negative and anaerobic bacteria:
Piperacillin-tazobactam
Ceftriaxone + Metronidazole
Carbapenems in severe cases
3. Biliary Drainage
Relieving the obstruction is crucial:
ERCP with sphincterotomy to remove stones or place stents
Percutaneous transhepatic cholangiography (PTC) if ERCP fails
Surgical decompression in rare cases
4. Supportive Care
IV fluids
Pain control
Antipyretics
Nutritional support
5. Long-term Management
For chronic or recurrent cholangitis:
Bile duct dilatation
Stent replacement
Liver transplantation in PSC or end-stage liver disease
Complications of Cholangitis
If untreated or inadequately managed, cholangitis can lead to serious complications:
Bile duct stricture
Cholangiohepatitis
Secondary biliary cirrhosis
Prevention of Cholangitis
1. Timely Treatment of Gallstones
Removing the gallbladder or stones before complications arise.
2. Safe ERCP Procedures
Performed by experienced specialists to avoid introducing infection.
3. Control of Underlying Conditions
Managing inflammatory bowel disease or autoimmune disorders can reduce risk.
4. Antibiotic Prophylaxis
Administered before ERCP in high-risk patients.
Living with Chronic Cholangitis
Patients with primary sclerosing cholangitis or recurrent infections need long-term follow-up. Regular imaging, liver function monitoring, and sometimes immunosuppressive therapy may be required. Avoiding alcohol, maintaining a balanced diet, and staying vaccinated (hepatitis A and B) are essential.
When to See a Doctor
Immediate medical attention is necessary if you experience:
Fever with chills
Yellowing of eyes or skin
Severe abdominal pain
Mental confusion or low blood pressure
These signs could indicate acute cholangitis requiring urgent treatment.
Cholangitis in Children
Though rare, cholangitis can affect children, particularly after biliary surgery or in congenital conditions like biliary atresia. Symptoms may be more subtle and include failure to thrive, pale stools, and irritability.
Cholangitis is a potentially life-threatening but treatable condition when diagnosed early. Awareness of symptoms like upper right abdominal pain, fever, jaundice, and dark urine is vital for timely medical intervention.
At Sparsh Diagnostic Centre, we offer comprehensive diagnostic tools including ultrasound, liver function testing, and imaging to help detect and manage cholangitis efficiently. Our experienced medical professionals ensure accurate diagnosis and timely referral for specialist treatment when needed.
If you’re experiencing symptoms of cholangitis, don’t wait. Early diagnosis can make all the difference.
Sparsh Diagnostic Centre:
📍 Centre Open:
Mon to Sat – 7 AM to 9 PM
Sunday – 7 AM to 3 PM
📞 Contact: 9830117733 / 8335049501
🌐 Visit: www.sparshdiagnostica.com
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()






[…] such as cholangitis, gallstones, and bile duct obstruction allow bacteria to travel into the liver and form an […]
[…] Primary biliary cholangitis […]