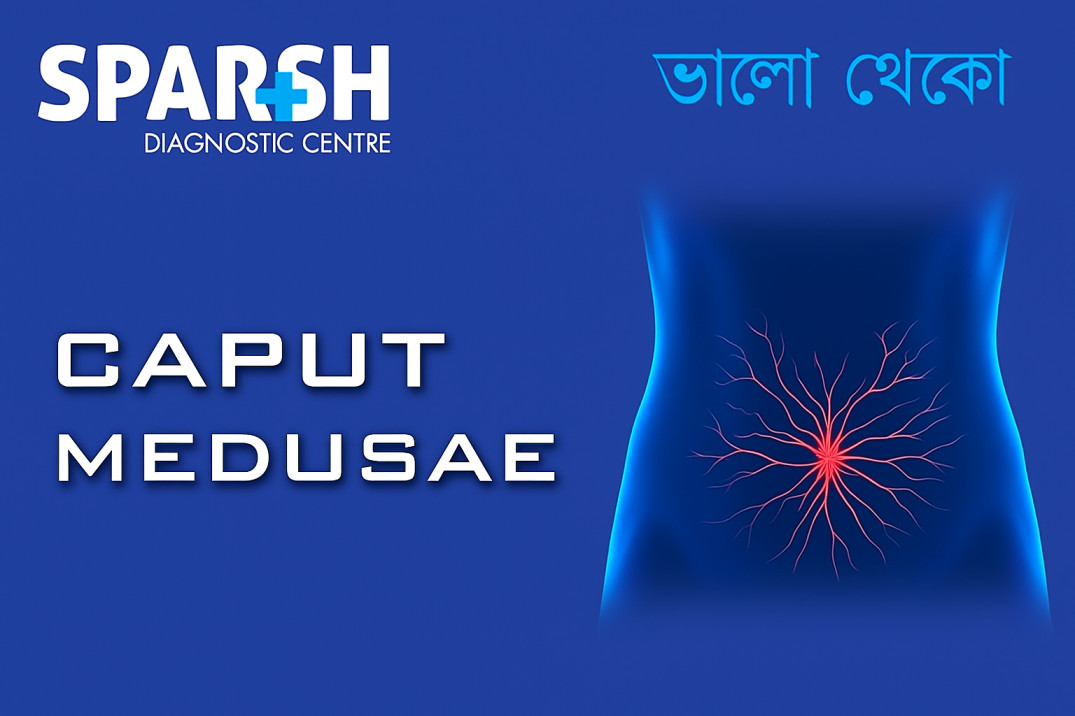
The human body often provides visible signs when something is wrong internally. One such striking sign is Caput Medusae — a medical term describing prominent, distended veins radiating from the navel (umbilicus) resembling the snake-covered head of Medusa from Greek mythology.
While the appearance itself might seem harmless, Caput Medusae is often a red flag for severe underlying liver disease, particularly portal hypertension, which indicates increased pressure in the portal venous system. Understanding the causes, associated conditions, and appropriate diagnostic and treatment approaches can help prevent further complications.
This blog explains what Caput Medusae means, its causes, symptoms, diagnosis, and management, along with preventive measures to protect liver health.
What Is Caput Medusae?
Caput Medusae refers to engorged and visible veins around the umbilicus, caused by obstruction or increased pressure in the portal venous system. The veins become dilated as blood seeks alternative pathways back to the heart, bypassing the high-pressure portal system.
These veins typically radiate outward from the navel like snakes — hence the term “Medusa’s head.” It is not a disease by itself but rather a clinical sign of portal hypertension, commonly associated with liver cirrhosis or other serious hepatic conditions.
Understanding the Connection Between the Liver and Caput Medusae
The portal vein carries blood from the stomach, intestines, spleen, and pancreas to the liver. The liver then filters toxins, stores nutrients, and processes metabolic products before sending the blood back to the heart.
When the liver is damaged — such as from cirrhosis, fibrosis, or thrombosis — blood cannot flow freely through it. The resulting back pressure in the portal vein leads to portal hypertension.
To relieve this pressure, the body develops collateral veins around the abdomen, particularly near the umbilicus. Over time, these veins enlarge and become visible on the abdominal wall — forming Caput Medusae.
Causes of Caput Medusae
Caput Medusae occurs due to increased portal venous pressure or blockage in the venous return from the abdominal organs. The most common causes include:
1. Liver Cirrhosis
Cirrhosis is the leading cause of Caput Medusae. Long-term liver damage from conditions like alcoholic liver disease, hepatitis B or C, or non-alcoholic fatty liver disease (NAFLD) leads to scar tissue formation. This fibrosis obstructs blood flow, resulting in portal hypertension.
2. Portal Vein Thrombosis
A blood clot in the portal vein prevents normal blood flow through the liver, forcing blood to reroute through superficial veins near the navel.
3. Budd-Chiari Syndrome
This rare condition involves obstruction of hepatic veins, which carry blood away from the liver. The backflow increases portal pressure, causing collateral vein formation.
4. Hepatic or Inferior Vena Cava Obstruction
Blockage in the inferior vena cava (the major vein returning blood from the lower body to the heart) can also lead to venous congestion and visible abdominal veins.
5. Schistosomiasis
In regions where parasitic infections like schistosomiasis are common, chronic inflammation can lead to liver fibrosis and portal hypertension.
6. Right-Sided Heart Failure
Severe heart failure may cause backflow of blood into the hepatic and abdominal veins, leading to congestion and the development of Caput Medusae.
Symptoms Associated with Caput Medusae
While the most obvious feature is the visible network of veins around the umbilicus, Caput Medusae rarely appears in isolation. It is usually accompanied by symptoms of chronic liver disease or portal hypertension, such as:
Prominent, snake-like veins radiating from the navel
Loss of appetite and weight loss
Easy bruising or bleeding (due to impaired clotting function)
Spider angiomas (small, spider-like blood vessels on skin)
Palmar erythema (reddening of palms)
If left untreated, complications like esophageal varices (swollen veins in the esophagus that can rupture and bleed) may occur — a life-threatening emergency.
How Is Caput Medusae Diagnosed?
The diagnosis of Caput Medusae involves clinical examination and imaging tests to confirm the presence of portal hypertension and identify the underlying cause.
1. Physical Examination
A physician inspects the abdomen for visible veins around the navel. The direction of blood flow in these veins helps distinguish Caput Medusae from other conditions:
Flow away from the umbilicus → Portal hypertension (true Caput Medusae)
Flow toward the umbilicus → Obstruction of inferior vena cava
2. Doppler Ultrasound
An abdominal Doppler ultrasound is the most common non-invasive test used to assess portal vein patency, blood flow direction, and the presence of collateral circulation.
3. CT Scan or MRI
These imaging modalities help visualize liver structure, portal system, and associated abnormalities like thrombosis or tumors.
4. Liver Function Tests (LFTs)
Blood tests check for elevated bilirubin, liver enzymes (ALT, AST), and albumin levels, which reflect the liver’s functional status.
5. Endoscopy
In some cases, an upper gastrointestinal endoscopy is performed to check for esophageal varices, another common sign of portal hypertension.
Treatment of Caput Medusae
Since Caput Medusae is a symptom, not a standalone disease, the treatment focuses on managing the underlying cause — typically portal hypertension and liver disease.
1. Treating the Underlying Liver Condition
For cirrhosis: Management includes alcohol cessation, antiviral therapy (for hepatitis), low-sodium diet, and diuretics to reduce fluid buildup.
For fatty liver disease: Lifestyle changes like weight loss, exercise, and blood sugar control help slow disease progression.
2. Medications to Reduce Portal Hypertension
Non-selective beta-blockers (e.g., propranolol, nadolol) help lower portal pressure and prevent variceal bleeding.
Vasodilators may be used to improve hepatic blood flow.
3. Endoscopic Therapy
If esophageal varices are present, endoscopic band ligation or sclerotherapy can prevent life-threatening bleeding.
4. Transjugular Intrahepatic Portosystemic Shunt (TIPS)
This minimally invasive procedure creates a channel between the portal and hepatic veins, allowing blood to bypass the scarred liver tissue and reduce portal pressure.
5. Surgical Intervention
In severe cases where other treatments fail, surgical portosystemic shunts or liver transplantation may be necessary.
6. Lifestyle Modifications
Follow a balanced diet rich in fruits, vegetables, and lean proteins.
Limit salt intake to prevent fluid retention.
Stay physically active and maintain a healthy weight.
Take medications strictly as prescribed by a doctor.
Complications of Caput Medusae
If the underlying liver disease is not managed properly, patients may develop severe complications such as:
Variceal bleeding (ruptured veins in the esophagus or stomach)
Ascites (fluid accumulation in the abdomen)
Hepatic encephalopathy (brain dysfunction due to liver failure)
Spontaneous bacterial peritonitis
Liver failure requiring transplantation
Early detection and proper treatment of the underlying cause are crucial to prevent these outcomes.
Prevention of Caput Medusae
While Caput Medusae itself cannot always be prevented, its root cause — liver disease and portal hypertension — often can.
Here are key preventive measures:
Avoid excessive alcohol consumption
Alcohol abuse is the leading cause of cirrhosis and liver failure.
Get vaccinated against Hepatitis B
Prevents one of the most common causes of chronic liver damage.
Practice safe hygiene and safe sex
Reduces risk of Hepatitis B and C transmission.
Maintain a healthy diet
A balanced, low-fat diet helps prevent fatty liver disease.
Exercise regularly
Keeps the liver healthy and reduces risk of metabolic syndrome.
Avoid unnecessary medications and toxins
Overuse of certain drugs or supplements can harm the liver.
Get regular health check-ups
Routine liver function tests and abdominal ultrasounds can detect problems early.
When to See a Doctor
Seek medical help immediately if you notice:
Prominent, dilated veins around your navel
Unexplained abdominal swelling
Jaundice (yellowing of skin/eyes)
Fatigue, loss of appetite, or unintentional weight loss
Vomiting blood or black stools
These may indicate advanced liver disease or portal hypertension — both of which require urgent evaluation.
Diagnosis and Management at Sparsh Diagnostic Centre
At Sparsh Diagnostic Centre, our team of experienced radiologists and hepatology experts provide comprehensive evaluation and imaging for conditions like Caput Medusae.
Our diagnostic services include:
Abdominal ultrasound and Doppler imaging
Liver function and blood tests
We ensure accurate diagnosis, early detection of complications, and close coordination with specialists for effective treatment and long-term management.
Frequently Asked Questions (FAQs)
1. Is Caput Medusae painful?
No, Caput Medusae itself is usually painless. However, the underlying liver disease may cause abdominal discomfort, swelling, or tenderness.
2. Is Caput Medusae reversible?
The veins may shrink once the underlying cause (like portal hypertension) is controlled. However, in advanced liver disease, the condition might persist until effective treatment or liver transplantation.
3. Can fatty liver cause Caput Medusae?
Yes, severe non-alcoholic steatohepatitis (NASH) or advanced fatty liver disease can lead to cirrhosis and portal hypertension, which may result in Caput Medusae.
4. How is Caput Medusae different from abdominal varicose veins?
Caput Medusae is due to portal hypertension (from liver disease), whereas varicose veins are caused by venous insufficiency in the legs or abdomen. The direction of blood flow differs in each.
5. What are the main treatments available for Caput Medusae?
Treatment focuses on managing portal hypertension and its cause — through medications, lifestyle changes, TIPS procedure, or liver transplantation in advanced cases.
6. Is Caput Medusae life-threatening?
Caput Medusae itself isn’t dangerous, but it signals serious underlying liver problems. Without timely treatment, complications like bleeding varices or liver failure can be life-threatening.
Caput Medusae is more than a cosmetic concern — it is a warning sign of serious liver disease and portal hypertension. Recognizing this early can help prevent severe complications like variceal bleeding or liver failure.
If you notice abnormal abdominal veins or other liver-related symptoms, seek professional evaluation immediately.
At Sparsh Diagnostic Centre, our advanced imaging facilities and expert diagnostics ensure accurate assessment and early intervention, helping you take control of your liver health.
👉 To book a liver health check-up, visit Sparsh Diagnostic Centre or call our helpline 9830117733 today.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()