Cellulitis is a common but potentially serious bacterial skin infection that affects the deeper layers of the skin and the underlying tissue. While it often begins as a small area of redness, it can quickly spread and cause severe illness if left untreated. Most cases of cellulitis affect the lower legs, but it can appear anywhere on the body, including the arms, face, and even the scalp.
Cellulitis requires prompt medical attention. In some cases, hospitalization may be necessary if the infection spreads rapidly, is accompanied by fever, or affects individuals with weakened immune systems.
This comprehensive guide explores everything you need to know about cellulitis — from its causes and risk factors to symptoms, diagnosis, and treatment options.
What is Cellulitis?
Cellulitis is a bacterial infection of the skin and subcutaneous tissues. The infection typically occurs when bacteria enter the skin through a break, cut, insect bite, or surgical wound.
The most common bacteria responsible are:
Streptococcus pyogenes
Staphylococcus aureus
In severe cases, cellulitis can spread through the bloodstream (bacteremia) and lead to sepsis, a life-threatening complication.
Causes of Cellulitis
Cellulitis usually develops when bacteria penetrate the skin barrier. The most common causes include:
Breaks in the skin – cuts, wounds, burns, or abrasions.
Insect bites or stings – which provide a pathway for bacteria.
Skin conditions – such as eczema, athlete’s foot, psoriasis, or shingles.
Surgical wounds – infections post-surgery can trigger cellulitis.
Animal bites or scratches – including cats and dogs.
Risk Factors for Cellulitis
Anyone can develop cellulitis, but certain factors increase the risk:
Weakened immune system (HIV, cancer treatment, diabetes).
Chronic skin conditions (eczema, athlete’s foot, ulcers).
Edema (swelling) due to lymphatic obstruction or venous insufficiency.
Obesity – linked to skin folds and poor circulation.
Previous cellulitis episodes – increases recurrence risk.
Poor circulation – including peripheral artery disease.
Symptoms of Cellulitis
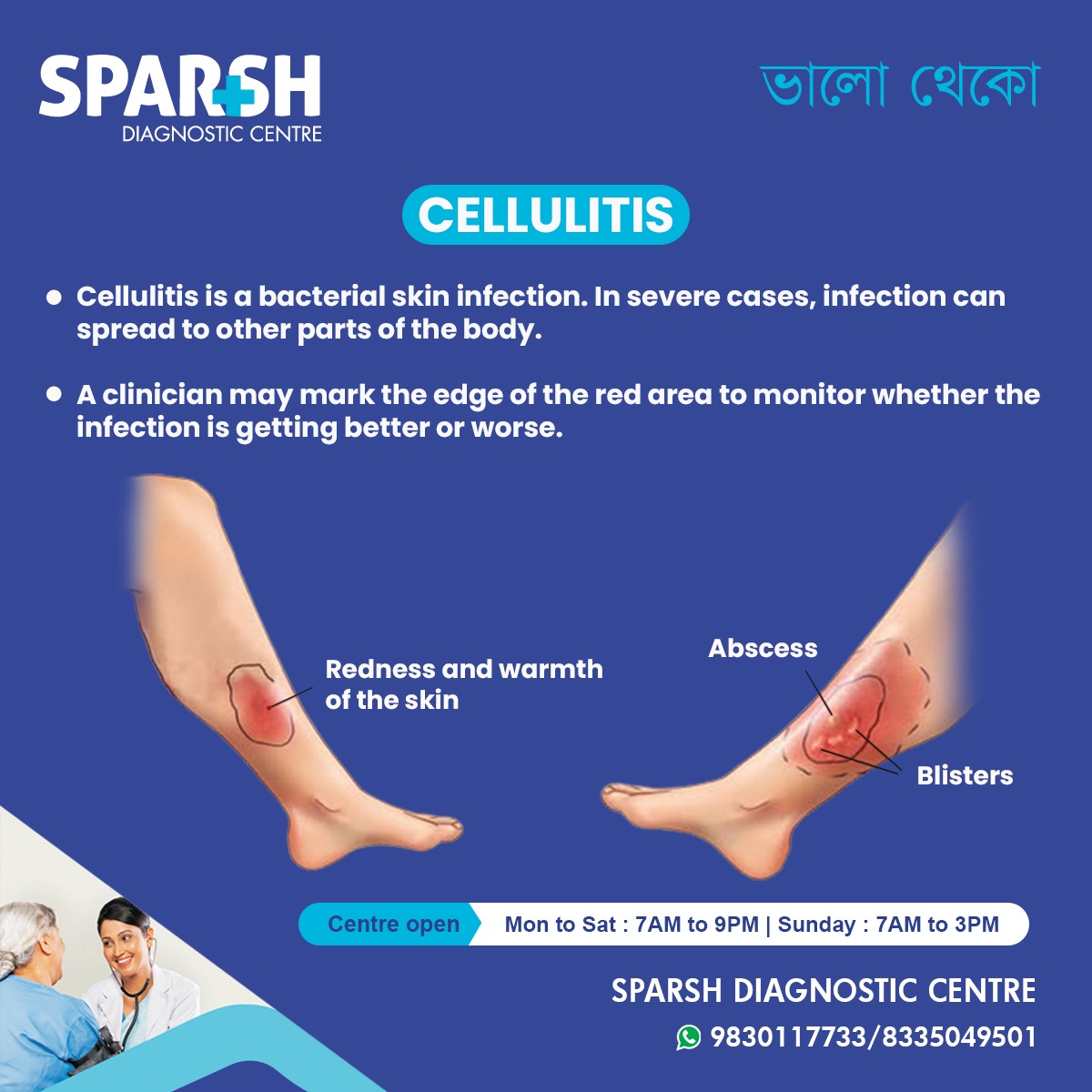
Cellulitis symptoms vary depending on severity but commonly include:
Redness of the skin
Warmth and tenderness in the affected area
Swelling (edema)
Pain in the infected region
Blisters or skin dimpling
Abscess formation (pus-filled pocket)
Systemic Symptoms (Advanced Infection)
If cellulitis spreads, systemic symptoms may appear, including:
These signs require immediate medical attention.
Complications of Cellulitis
Without timely treatment, cellulitis may lead to serious complications:
Abscess formation – pus accumulation requiring drainage.
Sepsis – life-threatening infection spreading throughout the body.
Osteomyelitis – infection spreading to the bone.
Gangrene – tissue death due to poor blood flow.
Lymphangitis – red streaks indicating infection in lymph vessels.
Chronic swelling (lymphedema) – recurrent cellulitis can damage lymphatic circulation.
Diagnosis of Cellulitis
A healthcare professional can usually diagnose cellulitis based on physical examination and medical history.
Steps in Diagnosis
Physical Exam – doctor inspects redness, swelling, and warmth.
Marking the skin – clinicians may outline the red area to track spread.
Blood Tests – to check for infection markers (white blood cell count).
Wound Culture – if pus or discharge is present.
Imaging Tests (Ultrasound, MRI, or CT scan) – in severe or recurrent cases to rule out deep infection or abscess.
Treatment of Cellulitis
1. Medications
Antibiotics – primary treatment (oral or IV depending on severity).
Mild cases: oral antibiotics for 7–14 days.
Severe cases: hospitalization with IV antibiotics.
Pain relievers – acetaminophen or ibuprofen for pain and fever.
2. Supportive Care
Rest and elevate the affected area.
Apply cool, damp cloths to reduce discomfort.
Keep skin clean and hydrated.
3. Surgical Intervention
In case of abscess formation, surgical drainage may be necessary.
Necrotic tissue may require debridement.
Prevention of Cellulitis
Preventive measures can significantly reduce risk:
Maintain good hygiene – wash hands regularly.
Moisturize skin – prevent dryness and cracking.
Treat wounds promptly – clean cuts and apply antiseptic.
Manage chronic skin conditions – eczema, athlete’s foot, psoriasis.
Wear protective clothing – especially if prone to insect bites.
Monitor swelling – patients with lymphedema should use compression therapy.
Prognosis of Cellulitis
With early diagnosis and appropriate treatment, most cases resolve completely within 7–14 days. However, severe or untreated cellulitis can lead to hospitalization, chronic recurrence, or even death in rare cases.
Living with Recurrent Cellulitis
Some individuals experience recurrent cellulitis, especially those with lymphedema or venous insufficiency. Preventive antibiotics may be prescribed for high-risk patients. Regular follow-up with a healthcare provider is essential.
Frequently Asked Questions (FAQ)
Q1. What is the main cause of cellulitis?
It is primarily caused by bacteria — most often Streptococcus pyogenes or Staphylococcus aureus — entering through a break in the skin.
Q2. How do you know if it is serious?
If you have spreading redness, fever, chills, blisters, or red streaks leading away from the infected area, it may be serious and requires immediate medical attention.
Q3. Can it heal on its own?
No, cellulitis usually requires antibiotic treatment. Without proper care, the infection can worsen and lead to severe complications.
Q4. How long does it take to heal?
Mild cellulitis improves within 7–14 days with antibiotics. Severe cases may take longer and require hospitalization.
Q5. Is it contagious?
Cellulitis itself is not contagious, but the bacteria that cause it can spread through direct contact if someone has open wounds.
Q6. Can it come back?
Yes, cellulitis can recur, especially in individuals with chronic swelling, skin conditions, or a history of multiple infections.
Q7. What is the difference between cellulitis and abscess?
Cellulitis is a diffuse bacterial infection of the skin, while an abscess is a localized pus-filled lump. Sometimes both can occur together.
Q8. Who is most at risk for cellulitis?
People with weakened immune systems, diabetes, obesity, poor circulation, or chronic skin conditions are more likely to develop cellulitis.
Cellulitis is a serious skin infection that requires timely diagnosis and treatment. While most cases can be successfully treated with antibiotics, complications can arise if neglected. Preventive care — such as proper wound management, good hygiene, and managing chronic skin conditions — plays a crucial role in reducing the risk.
At Sparsh Diagnostic Centre, we are committed to providing comprehensive care and accurate diagnostic testing to help you stay healthy and prevent complications of infections like cellulitis.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()






[…] infections – Cellulitis, abscesses, or […]
[…] Infections: Chronic swelling can cause the skin to become fragile and prone to infections, such as cellulitis. Open sores or ulcers may also develop, particularly in the […]
[…] Skin infections, including cellulitis or infections caused by wounds, can result in the […]
[…] Spread: Infections from nearby tissues, such as cellulitis or an infected diabetic foot ulcer, can extend to the […]