Whipple’s Disease is a rare, systemic infectious disorder that primarily affects the small intestine but can also impact the joints, heart, brain, and other organs. Caused by the bacterium Tropheryma whipplei, this condition can become life-threatening if left untreated. Though uncommon, timely recognition and treatment are critical for preventing serious complications.
In this in-depth article, we’ll explore the causes, symptoms, risk factors, diagnostic approaches, and treatment options for Whipple’s Disease, helping you understand the importance of early medical intervention.
What is Whipple’s Disease?
Whipple’s Disease is a chronic multisystem disorder caused by infection with the gram-positive bacterium Tropheryma whipplei. It predominantly affects the gastrointestinal (GI) tract, leading to malabsorption — a condition where the body is unable to absorb nutrients properly.
The disease can also involve other organ systems, resulting in a wide range of symptoms including joint pain, neurological issues, cardiac manifestations, and skin abnormalities. Because of its varied presentation and rarity, Whipple’s Disease is often misdiagnosed or diagnosed late.
Epidemiology: How Common is It?
Whipple’s Disease is extremely rare, with an estimated incidence of less than 1 in 1,000,000 people annually. It affects middle-aged Caucasian men more commonly than other groups, though it can occur in individuals of any age, gender, or ethnicity.
Causes: What Triggers Whipple’s Disease?
The disease is caused by infection with Tropheryma whipplei, a bacterium found in soil and sewage. Most people exposed to this bacterium do not develop the disease, suggesting that host immune factors play a crucial role in its pathogenesis.
Some individuals may have a genetic predisposition or immune deficiency that impairs their ability to clear the bacteria, allowing it to proliferate and spread throughout the body.
Transmission: How Does It Spread?
The exact mode of transmission is not clearly understood, but it is believed to occur via fecal-oral route, particularly through contaminated water or food. Person-to-person transmission is considered extremely rare.
Risk Factors
While Whipple’s Disease is rare, several factors may increase susceptibility:
Caucasian ethnicity
Occupational exposure to sewage or soil
Immunosuppression
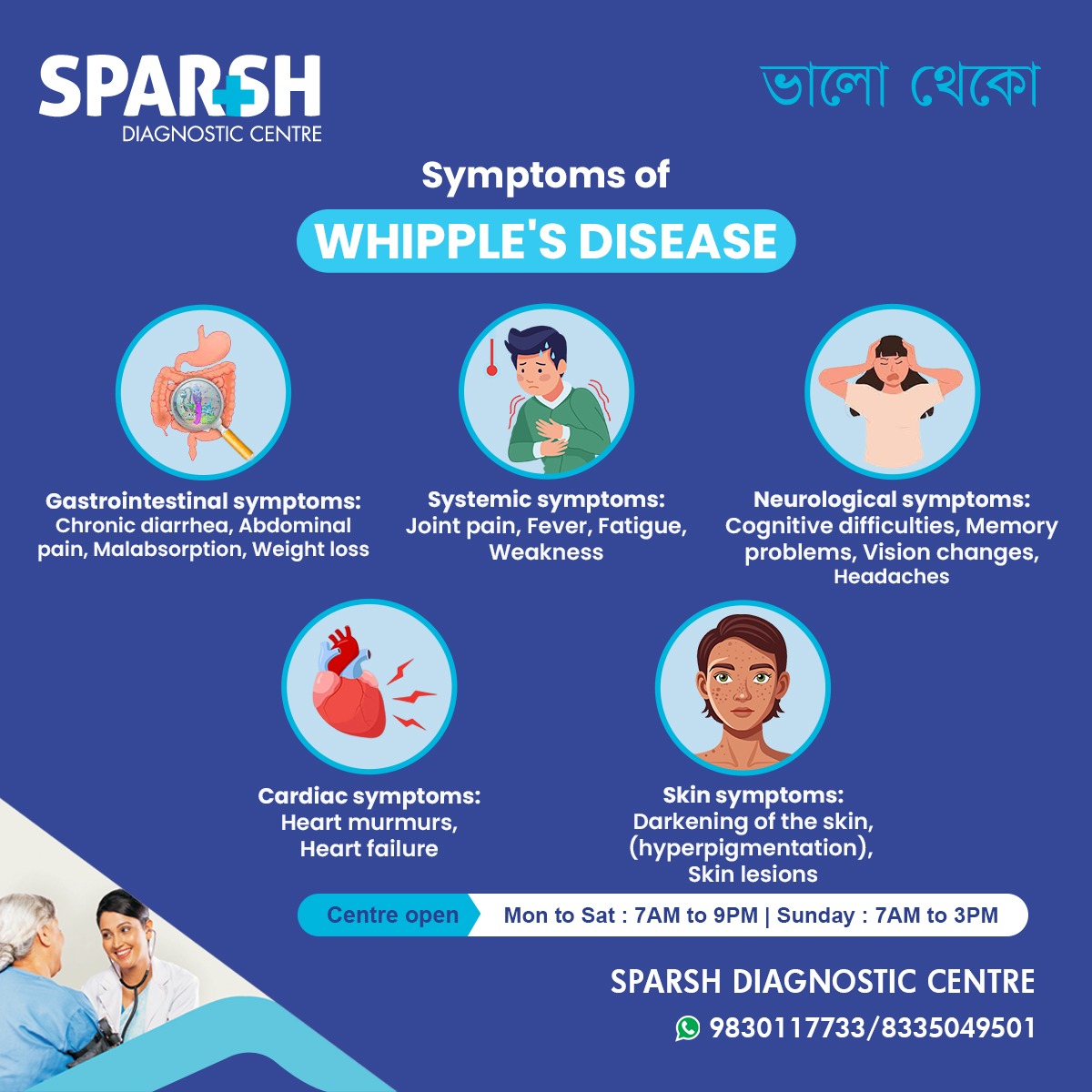
Symptoms of Whipple’s Disease
Whipple’s Disease presents a multisystemic array of symptoms, which often makes diagnosis challenging. Symptoms usually develop gradually and may persist for years before a correct diagnosis is made.
1. Gastrointestinal Symptoms
These are the most common and typically the earliest to appear:
These symptoms arise due to damage to the small intestinal mucosa, impairing nutrient absorption.
2. Systemic Symptoms
Joint pain (arthralgia) – often migratory and non-destructive
Weakness
Systemic signs often precede gastrointestinal complaints by months or years.
3. Neurological Symptoms
Neurological involvement can occur in up to 40% of untreated cases and may include:
Cognitive difficulties
Memory problems
Vision changes (including nystagmus and visual loss)
Headaches
Dementia-like symptoms
Myoclonus
Oculomasticatory myorhythmia (a rare, pathognomonic finding)
4. Cardiac Symptoms
Cardiac involvement, though less common, can be serious:
Whipple’s endocarditis may occur without fever and can mimic culture-negative infective endocarditis.
5. Skin Symptoms
Hyperpigmentation (especially on sun-exposed areas)
Skin lesions or nodules
These skin manifestations may be linked to nutritional deficiencies or direct bacterial involvement.
Complications of Untreated Whipple’s Disease
If left untreated, Whipple’s Disease can lead to:
Neurological damage
Coma
Cardiac failure
Death
The condition is potentially fatal, but treatment usually leads to dramatic improvement.
Diagnosis of Whipple’s Disease
Diagnosing Whipple’s Disease involves a combination of clinical suspicion, histopathological evaluation, and molecular tests.
1. Clinical History and Physical Exam
Physicians evaluate symptoms such as:
Chronic diarrhea
Weight loss
Arthralgia
Neurological complaints
Fever of unknown origin
2. Laboratory Tests
CBC may show anemia
Serum albumin may be low
Inflammatory markers (CRP, ESR) may be elevated
3. Endoscopy and Biopsy
Upper GI endoscopy allows visualization and biopsy of the small intestine.
PAS-positive macrophages in intestinal biopsies are a hallmark finding.
Electron microscopy may show bacillary structures in macrophages.
4. PCR Testing
Polymerase chain reaction (PCR) testing can detect T. whipplei DNA in various tissues including intestinal biopsy samples, CSF, and blood.
5. Imaging
MRI or CT scans may be used to evaluate neurological involvement.
Echocardiography is useful for assessing cardiac complications.
Differential Diagnosis
Due to its nonspecific and overlapping symptoms, Whipple’s Disease is often confused with:
Correct diagnosis requires a high index of suspicion and confirmatory testing.
Treatment of Whipple’s Disease
Whipple’s Disease is highly treatable, especially when diagnosed early. Antibiotic therapy is the cornerstone of treatment.
1. Initial Phase (Induction Therapy)
IV ceftriaxone or penicillin + streptomycin for 2 weeks to ensure penetration into the CNS and other tissues.
2. Maintenance Phase (Oral Therapy)
Followed by oral trimethoprim-sulfamethoxazole (TMP-SMX) for 12 months.
Alternatives: Doxycycline + hydroxychloroquine for 12-18 months.
The prolonged course is essential to prevent relapse, especially in neurological and cardiac involvement.
Monitoring and Follow-Up
Patients require regular follow-up with clinical evaluations, lab tests, and sometimes repeat PCR testing.
Recurrence can occur and may require retreatment or alternative regimens.
Prognosis
With appropriate treatment, the prognosis is excellent. Most patients experience a dramatic improvement within weeks of starting antibiotics. However, delayed diagnosis or incomplete treatment may result in permanent organ damage or death.
Prevention
Since the exact mode of transmission is unclear and T. whipplei is ubiquitous, there are no specific preventive measures. However, general recommendations include:
Good hygiene practices
Avoiding contaminated water and food
Prompt medical attention for unexplained gastrointestinal or systemic symptoms
FAQs About Whipple’s Disease
1. Can Whipple’s Disease recur?
Yes, especially if treatment is stopped prematurely. Lifelong monitoring is often necessary.
2. Is Whipple’s Disease contagious?
No, it is not considered contagious between humans.
3. Can it be cured?
Yes, with appropriate long-term antibiotic treatment, most cases can be completely cured.
4. How long does it take to recover?
Symptoms often improve within a few weeks, but full recovery may take months to a year depending on the severity and organs involved.
Whipple’s Disease, though rare, is a serious and potentially fatal condition if not diagnosed and treated in time. The disease’s multisystem nature — affecting the gut, joints, brain, heart, and skin — demands a high level of clinical awareness.
Early diagnosis through biopsy and PCR testing, followed by prolonged antibiotic therapy, is the key to effective management and cure. Patients experiencing unexplained weight loss, chronic diarrhea, joint pain, or neurological symptoms should consult a healthcare provider promptly.
If you or a loved one is experiencing unexplained systemic or gastrointestinal symptoms, reach out to Sparsh Diagnostic Centre for accurate testing and compassionate care.
Sparsh Diagnostic Centre
🌐 www.sparshdiagnostica.com
📍 Bansdroni, Kolkata
📞 9830117733 / 8335049501
🕒 Mon to Sat: 7 AM – 9 PM | Sunday: 7 AM – 3 PM
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()






[…] Whipple’s disease – Rare bacterial infection affecting the intestinal lining. […]