Leukostasis is rare, but when it happens, it’s extremely serious. It occurs when the white blood cell (WBC) count rises to dangerously high levels — most commonly in people with acute leukemia. In these situations, it becomes a true medical emergency.
When white blood cells build up excessively, they don’t just circulate normally. They can become thick and sticky, slowing down blood flow and blocking tiny blood vessels. As a result, vital organs like the brain and lungs may not get enough oxygen. Without urgent treatment, this can lead to breathing failure, stroke-like symptoms, or even death.
In this guide, we’ll walk through what leukostasis is, why it happens, the symptoms to watch for, and how it’s treated — in clear, practical terms.
What Exactly Is Leukostasis?
Leukostasis happens when very high numbers of abnormal white blood cells interfere with normal blood flow. Doctors often see it when WBC counts climb above 100,000/µL, though symptoms can sometimes appear at lower levels.
In simple terms, leukostasis involves:
Extremely elevated white blood cell counts
Clumping of immature leukemia cells (called blasts) in small blood vessels
Poor circulation in tiny vessels (microcirculation)
Reduced oxygen delivery to tissues
Organ dysfunction
It is most often linked to:
Acute Myeloid Leukemia (AML)
Acute Lymphoblastic Leukemia (ALL), though less commonly
What makes leukostasis so dangerous is how quickly it can damage organs — sometimes within hours.
Why Does Leukostasis Happen?
The main trigger is hyperleukocytosis — an abnormally high white blood cell count. But it’s not just about numbers. The type and behavior of the cells matter too.
In acute leukemia:
The white blood cells are immature (blast cells).
These blast cells are larger than normal.
They’re less flexible.
They tend to stick together.
When too many of these bulky, sticky cells circulate in the blood, they can clog small vessels. This thickens the blood and reduces oxygen flow to tissues.
The organs most commonly affected are:
Brain
Lungs
Heart
Retina (back of the eye)
Skin
Without rapid treatment, multiple organs can begin to fail.
Who Is at Higher Risk?
Certain patients are more likely to develop leukostasis, including those with:
Newly diagnosed acute leukemia
WBC counts above 100,000/µL
AML, especially the monocytic subtype
Delayed treatment for leukemia
Severe dehydration
Tumor lysis syndrome
AML patients are particularly vulnerable because AML blast cells are larger and more viscous compared to those in ALL.
Symptoms of Leukostasis
The symptoms depend on which organs are affected. Most often, the brain and lungs are involved first.
1. Brain (Neurological Symptoms)
When blood flow to the brain is impaired, symptoms can look very similar to a stroke. These may include:
Blurred vision or vision loss
Confusion
Difficulty walking (gait instability)
Cranial nerve problems
Drowsiness
Stupor
Coma
Weakness or numbness on one side of the body
These symptoms can worsen quickly, so immediate evaluation is critical.
2. Lungs (Respiratory Symptoms)
If leukostasis affects the lungs, it can become life-threatening very fast. Symptoms may include:
Low oxygen levels
Bleeding in the lungs (alveolar hemorrhage)
Some patients may need oxygen support or even mechanical ventilation.
3. Heart (Cardiovascular Symptoms)
Though less common, reduced blood flow to the heart can cause:
Chest pain
Even though this is rarer, it can be extremely serious.
4. Eyes
The retina can also be affected, leading to:
Visual disturbances
Retinopathy
5. Skin and Circulation
Poor blood flow to peripheral tissues may cause:
Skin mottling
Reduced circulation (hypoperfusion)
Tissue ischemia
Venous thrombosis
6. Other Symptoms
Some people may also experience:
Weakness
Altered mental status
Because leukostasis can resemble a stroke or severe infection, it’s easy to misinterpret early symptoms. That’s why awareness is so important.

How Is Leukostasis Diagnosed?
Leukostasis is mainly a clinical diagnosis, meaning doctors rely on symptoms along with lab results.
Complete Blood Count (CBC)
WBC count is often above 100,000/µL
Immature blast cells are present
However, symptoms can sometimes appear at lower counts, particularly in AML.
Peripheral Blood Smear
A closer look at the blood under a microscope shows:
Large numbers of immature blast cells
Abnormal cell shapes and features
Imaging
If neurological symptoms are present, doctors may order:
If breathing issues occur:
Chest X-ray or CT scan
These tests help rule out stroke, bleeding, or infection.
Bone Marrow Examination
This confirms the underlying diagnosis of leukemia.
Leukostasis vs. Hyperleukocytosis: What’s the Difference?
It’s easy to confuse the two.
Hyperleukocytosis simply means a very high white blood cell count.
Leukostasis refers to the symptoms and organ damage caused by that high count.
Not everyone with hyperleukocytosis develops leukostasis. But everyone with leukostasis has an elevated white blood cell count.
Is Leukostasis a Medical Emergency?
Absolutely.
Leukostasis is considered an oncologic emergency because:
Organ damage can happen quickly.
The risk of death is significant without treatment.
Delays worsen outcomes.
Patients usually require immediate hospital admission, often in an intensive care setting.
How Is Leukostasis Treated?
The main goal is simple but urgent: lower the white blood cell count quickly and restore proper blood flow.
1. Leukapheresis
Leukapheresis is a procedure that filters excess white blood cells out of the bloodstream. It can:
Rapidly lower WBC levels
Provide temporary relief
Stabilize patients with severe symptoms
It’s often used in cases involving brain or lung symptoms.
2. Cytoreductive Chemotherapy
This is the definitive treatment. Chemotherapy targets the underlying leukemia.
Common approaches include:
Hydroxyurea for rapid initial reduction
Induction chemotherapy for AML or ALL
Treatment must begin urgently.
3. Aggressive Hydration
IV fluids help:
Thin the blood
Improve circulation
Prevent tumor lysis syndrome
4. Preventing Tumor Lysis Syndrome
When cancer cells break down rapidly, complications can occur. Medications such as:
Allopurinol
Rasburicase
Help reduce this risk.
5. Supportive Care
Depending on severity, patients may need:
Oxygen therapy
Mechanical ventilation
ICU monitoring
Careful use of blood transfusions
Red blood cell transfusions are given cautiously, as they can increase blood viscosity.
Possible Complications
Without treatment, leukostasis can lead to:
Death
The good news is that early intervention greatly improves survival.
What Is the Prognosis?
Outcomes depend on several factors:
How quickly treatment begins
Type of leukemia
Age of the patient
Organs involved
Overall health
Mortality rates in severe cases may range from 20–40%, especially when respiratory failure develops. However, rapid leukapheresis and chemotherapy can significantly improve survival.
Can Leukostasis Be Prevented?
Prevention centers around early leukemia management:
Prompt evaluation of high WBC counts
Starting treatment early
Maintaining adequate hydration
Close monitoring of high-risk AML patients
Oncologists routinely track white blood cell counts to prevent this complication from developing.
When Should You Seek Emergency Care?
If someone with known or suspected leukemia develops:
Sudden confusion
Severe headache
Blurred vision
Shortness of breath
Chest pain
Weakness on one side of the body
They need immediate medical attention. These may be signs of leukostasis or a stroke-like complication.
Key Takeaways
Leukostasis is a life-threatening complication of extremely high white blood cell counts.
It most commonly occurs in acute myeloid leukemia.
The brain and lungs are affected most often.
Symptoms can resemble a stroke or severe respiratory illness.
It requires emergency treatment.
Leukapheresis and chemotherapy are the main therapies.
Early treatment saves lives.
Frequently Asked Questions (FAQ)
1. At what WBC count does leukostasis occur?
It often happens when WBC counts exceed 100,000/µL, though symptoms can appear at lower levels in AML.
2. Is leukostasis the same as leukemia?
No. Leukemia is a blood cancer. Leukostasis is a dangerous complication caused by extremely high white blood cell counts.
3. Can leukostasis cause a stroke?
Yes. It can block blood flow in the brain and cause stroke-like symptoms.
4. How quickly can leukostasis develop?
It can develop rapidly — sometimes within hours — especially in newly diagnosed acute leukemia.
5. Is leukostasis reversible?
Yes, if treated quickly. Delays can result in permanent organ damage.
6. Does every patient need leukapheresis?
Not always. It’s usually reserved for severe cases with neurological or respiratory symptoms. Chemotherapy is the definitive treatment.
7. What is the mortality rate?
Severe cases may have mortality rates of 20–40%, particularly when lung or brain involvement occurs.
8. Which type of leukemia is most associated with leukostasis?
Acute Myeloid Leukemia (AML).
9. Can it happen in chronic leukemia?
Rarely, but it can occur during blast crisis.
10. How can it be prevented?
Through early leukemia treatment, close monitoring of WBC counts, and rapid intervention when levels rise sharply.
Leukostasis is rare, but when it occurs, it moves fast and can be deadly. Because its symptoms often resemble a stroke or severe infection, it can be missed in the early stages.
Recognizing the warning signs and seeking immediate medical care can make the difference between recovery and serious complications. Quick diagnosis, urgent treatment, and aggressive management of the underlying leukemia are essential.
If you or someone you know with leukemia develops sudden breathing problems or neurological symptoms, treat it as an emergency.
Acting quickly can save a life.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
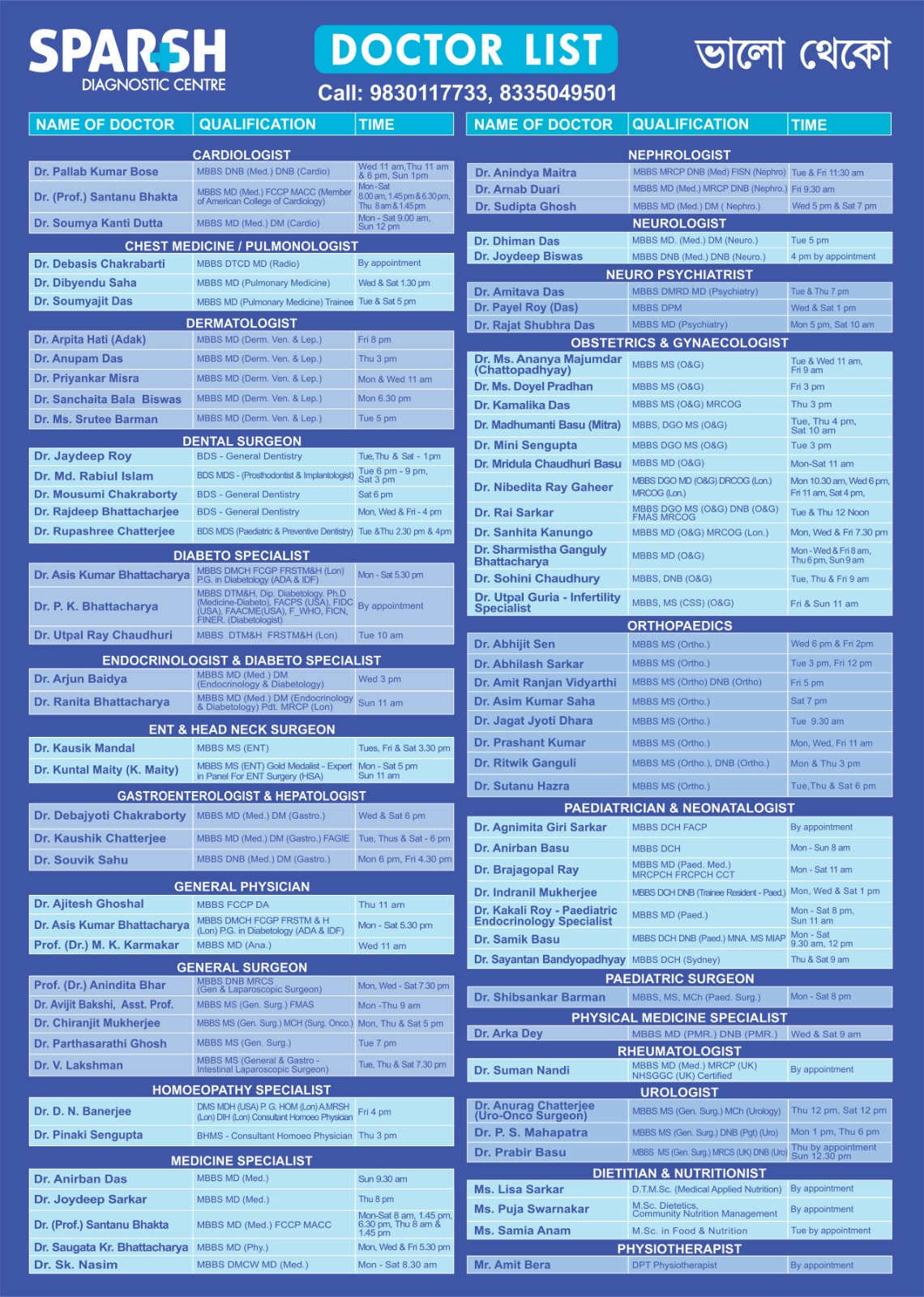
Sparsh Diagnostic Centre Doctor List
![]()





