Hypovolemic shock is a life-threatening medical emergency that occurs when the body loses a significant amount of blood or fluids, leading to inadequate circulation and oxygen delivery to vital organs. If not recognized and treated promptly, hypovolemic shock can rapidly progress to organ failure and death.
Understanding the causes, warning signs, diagnostic methods, and treatment options is essential for early intervention and improved survival outcomes.
What Is Hypovolemic Shock?
It is a type of shock caused by severe intravascular volume depletion. This depletion may result from:
Blood loss (hemorrhagic shock)
Loss of plasma or body fluids (non-hemorrhagic shock)
When circulating volume decreases, the heart cannot pump sufficient blood to tissues, resulting in reduced oxygen delivery and impaired cellular metabolism.
Types of Hypovolemic Shock
1. Hemorrhagic
Occurs due to significant blood loss, commonly caused by:
Trauma or accidents
Gastrointestinal bleeding
Surgical complications
Severe postpartum hemorrhage
2. Non-Hemorrhagic
Results from fluid loss without blood loss, such as:
Burns causing plasma leakage
Excessive sweating
Causes of Hypovolemic Shock
Common Causes Include:
Road traffic accidents
Internal bleeding
Severe infections with fluid loss
Burns covering large body areas
Kidney disorders causing excessive urination
Use of diuretics in excess
Pathophysiology: How does it develop
Loss of circulating volume
Decreased venous return to the heart
Reduced cardiac output
Inadequate tissue perfusion
Cellular hypoxia and metabolic acidosis
Multi-organ dysfunction
The body initially compensates by increasing heart rate and constricting blood vessels, but prolonged shock overwhelms these mechanisms.
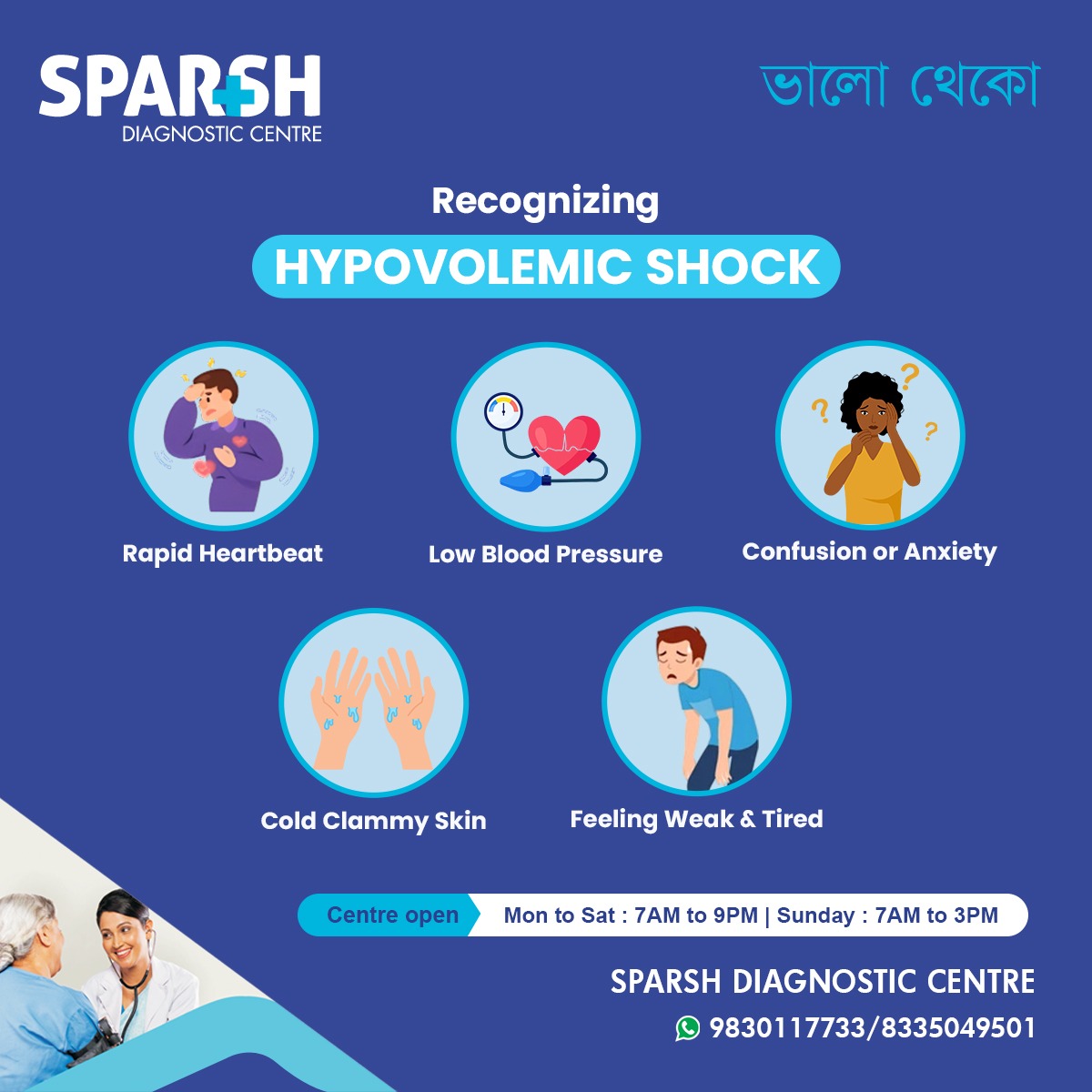
Signs and Symptoms of Hypovolemic Shock
Early recognition is critical. Symptoms may vary depending on severity and cause.
Early Symptoms:
Increased breathing rate
Pale or cool skin
Thirst
Anxiety or restlessness
Advanced Symptoms:
Confusion or altered mental state
Cold, clammy skin
Reduced urine output
Weak pulse
Loss of consciousness
Stages of Hypovolemic Shock
Stage 1 (Mild)
<15% fluid loss
Slight anxiety
Normal blood pressure
Stage 2 (Moderate)
15–30% fluid loss
Narrow pulse pressure
Stage 3 (Severe)
30–40% fluid loss
Marked hypotension
Mental confusion
Stage 4 (Critical)
40% fluid loss
Diagnosis of Hypovolemic Shock
Prompt diagnosis relies on clinical assessment and investigations.
Clinical Evaluation:
Vital signs (blood pressure, pulse, respiratory rate)
Mental status
Urine output
Skin temperature and capillary refill
Laboratory Tests:
Serum electrolytes
Blood urea and creatinine
Arterial blood gases
Lactate levels
Coagulation profile
Imaging Studies:
Treatment of Hypovolemic Shock
Management focuses on rapid restoration of circulating volume and treatment of the underlying cause.
1. Immediate Emergency Care
Ensure airway and oxygenation
Secure intravenous access
Monitor vital signs continuously
2. Fluid Resuscitation
Isotonic crystalloids (normal saline or Ringer’s lactate)
Colloids in selected cases
3. Blood Transfusion
Packed red blood cells
Plasma and platelets if massive hemorrhage
4. Control of Bleeding
Surgical intervention
Endoscopic procedures
Interventional radiology
5. Medications
Vasopressors (only after adequate fluid resuscitation)
Antibiotics if infection is suspected
Complications of Hypovolemic Shock
If treatment is delayed, complications may include:
Death
Prevention of Hypovolemic Shock
Preventive strategies include:
Prompt treatment of dehydration
Early management of bleeding
Adequate hydration during illness
Safe surgical practices
Trauma prevention measures
When to Seek Emergency Medical Care
Seek immediate medical attention if someone experiences:
Severe bleeding
Fainting or collapse
Sudden drop in blood pressure
Confusion with cold, clammy skin
Early intervention saves lives.
Role of Sparsh Diagnostic Centre in managing shock
Diagnostic centres play a vital role by providing:
Rapid blood tests
Imaging for internal bleeding
Monitoring support by renowned doctors
Early diagnosis of underlying causes
Timely diagnostics significantly improve outcomes in hypovolemic shock.
Frequently Asked Questions (FAQs)
What is the most common cause of hypovolemic shock?
Severe blood loss due to trauma or internal bleeding is the most common cause.
Is it reversible?
Yes, if identified and treated promptly, hypovolemic shock is reversible.
How fast can it develop?
It can develop within minutes to hours, especially after trauma or severe bleeding.
Can dehydration alone cause hypovolemic shock?
Yes, severe dehydration from diarrhea, vomiting, or heat exposure can lead to hypovolemic shock.
What is the first treatment for hypovolemic shock?
Rapid fluid resuscitation with intravenous fluids is the first line of treatment.
Is it fatal?
It can be fatal if untreated, but early recognition and intervention greatly improve survival.
Who is at higher risk?
Elderly individuals, trauma patients, surgical patients, and those with chronic illnesses are at higher risk.
How is it different from septic shock?
Hypovolemic shock is caused by fluid loss, whereas septic shock is caused by severe infection and inflammation.
Hypovolemic shock is a medical emergency requiring immediate attention. Awareness of its causes, early warning signs, and treatment options is crucial for saving lives. Rapid diagnosis, aggressive fluid resuscitation, and addressing the underlying cause form the cornerstone of management.
Timely access to emergency care and diagnostic services can make the difference between recovery and life-threatening complications.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

Sparsh Doctor List
![]()