Blood plays a vital role in keeping the body healthy, and one of its most important components is platelets. Platelets help stop bleeding by forming clots at the site of injury. When the platelet count falls below normal, the condition is known as thrombocytopenia.
Thrombocytopenia can range from mild and symptom-free to severe and life-threatening, depending on the underlying cause and how low the platelet count drops. Understanding this condition helps in early detection, timely treatment, and prevention of complications such as excessive bleeding.
This blog explains thrombocytopenia in simple terms, covering its causes, symptoms, diagnosis, treatment options, and commonly asked questions.
What Is Thrombocytopenia?
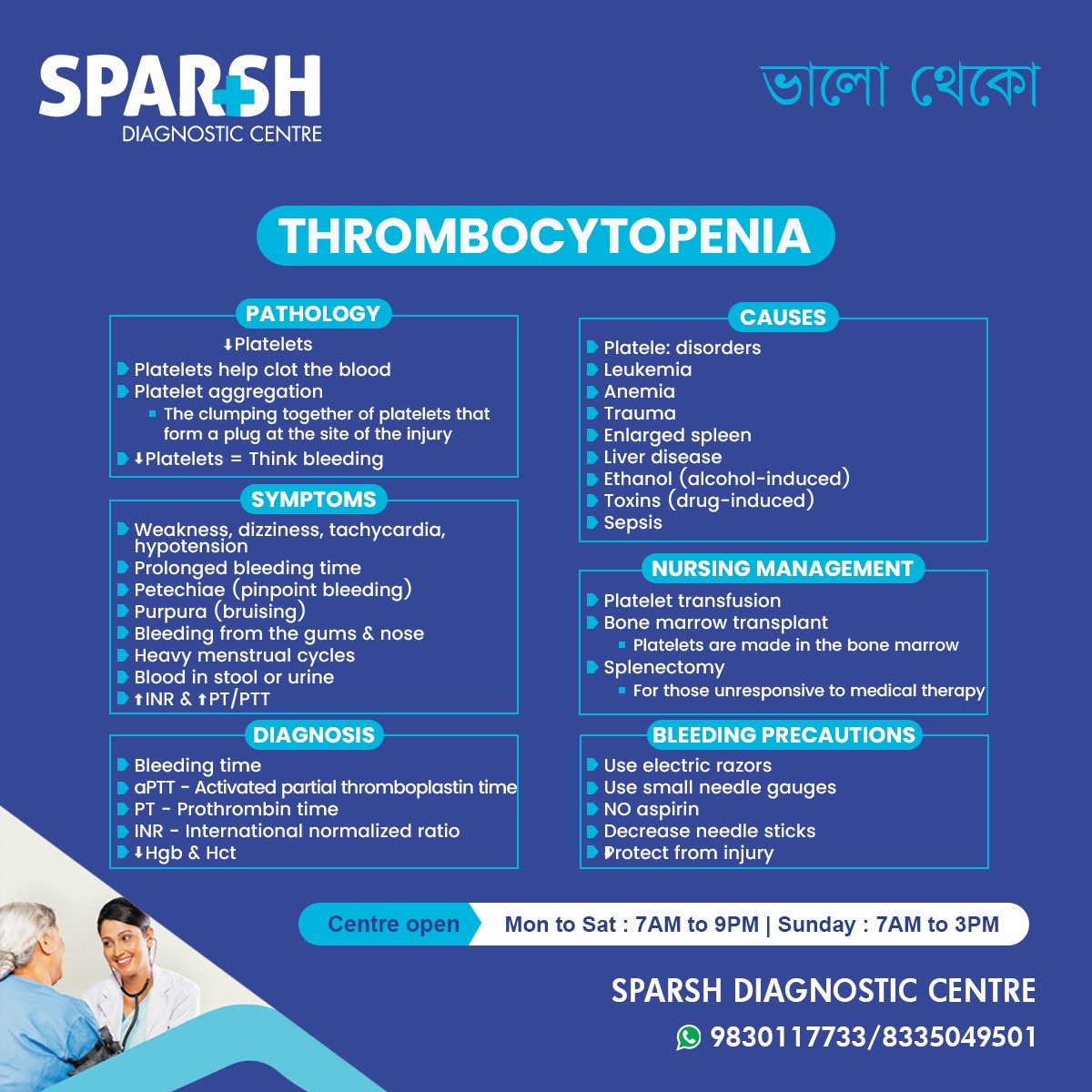
Thrombocytopenia is a blood disorder characterized by a low platelet count.
Normal platelet count: 150,000 to 450,000 platelets per microliter of blood
Thrombocytopenia is diagnosed when platelet levels fall below 150,000
Platelets are produced in the bone marrow and circulate in the blood, helping form clots whenever a blood vessel is damaged. A deficiency in platelets increases the risk of bleeding, both internally and externally.
Role of Platelets in the Body
Platelets are essential for:
Blood clot formation
Preventing excessive bleeding
Healing wounds and injuries
When a blood vessel is damaged:
Platelets rush to the site
They clump together (platelet aggregation)
A temporary plug is formed
Clotting factors strengthen the clot
Low platelet levels disrupt this process, making it difficult for the body to control bleeding.
Types of Thrombocytopenia
Thrombocytopenia can be classified based on the underlying mechanism:
1. Decreased Platelet Production
Occurs when the bone marrow does not produce enough platelets.
2. Increased Platelet Destruction
Platelets are destroyed faster than they are produced.
3. Platelet Sequestration
Platelets get trapped in an enlarged spleen.
Causes of Thrombocytopenia
Thrombocytopenia is not a disease itself but a sign of an underlying condition.
Bone Marrow Disorders
Aplastic anemia
Myelodysplastic syndromes
Bone marrow suppression due to chemotherapy or radiation
Immune-Related Causes
Immune thrombocytopenic purpura (ITP)
Autoimmune diseases like lupus
Drug-induced immune reactions
Infections
Liver and Spleen Disorders
Medications and Toxins
Alcohol (ethanol-induced)
Certain antibiotics
Chemotherapy drugs
Anti-seizure medications
Heparin (heparin-induced thrombocytopenia)
Other Causes
Trauma
Massive blood loss
Pregnancy-related conditions
Nutritional deficiencies (vitamin B12 or folate)
Symptoms of Thrombocytopenia
Symptoms depend on how low the platelet count is.
Mild Thrombocytopenia
Often asymptomatic
Discovered incidentally during routine blood tests
Moderate to Severe Thrombocytopenia
Prolonged bleeding from cuts
Nosebleeds
Bleeding gums
Heavy or prolonged menstrual periods
Blood in urine or stool
Low blood pressure in severe cases
Life-Threatening Signs
Internal bleeding
Bleeding in the brain
Black tarry stools
Immediate medical attention is required if severe bleeding occurs.
How Thrombocytopenia Is Diagnosed
Complete Blood Count (CBC)
Confirms low platelet count
May show low hemoglobin and hematocrit if bleeding is present
Peripheral Blood Smear
Examines platelet size and shape
Helps identify abnormal cells
Coagulation Tests
PT (Prothrombin Time)
aPTT (Activated Partial Thromboplastin Time)
INR (International Normalized Ratio)
Bone Marrow Examination
Done if bone marrow disease is suspected
Assesses platelet production
Additional Tests
Viral markers
Autoimmune screening
Vitamin B12 and folate levels
Platelet Count Levels and Bleeding Risk
| Platelet Count | Risk Level |
|---|---|
| 100,000–150,000 | Usually no symptoms |
| 50,000–100,000 | Mild bleeding risk |
| 20,000–50,000 | Moderate risk |
| Below 20,000 | High risk of spontaneous bleeding |
Treatment of Thrombocytopenia
Treatment depends on:
Severity of platelet drop
Underlying cause
Presence of bleeding
Observation
Mild cases may not require treatment
Regular monitoring of platelet count
Treating the Underlying Cause
Stopping offending drugs
Treating infections
Managing liver disease
Correcting nutritional deficiencies
Medications
Corticosteroids for immune-related causes
Immunoglobulin therapy
Immunosuppressive drugs
Platelet Transfusion
Used in severe cases
Given before surgery or during active bleeding
Bone Marrow Transplant
Considered in severe bone marrow failure disorders
Splenectomy
Removal of spleen in patients unresponsive to medical therapy
Reduces platelet destruction
Nursing and Supportive Management
Monitor for signs of bleeding
Avoid unnecessary injections
Use soft toothbrushes
Avoid rectal temperatures
Encourage rest
Maintain hydration
Bleeding Precautions for Patients
Patients with thrombocytopenia should:
Use electric razors instead of blades
Avoid aspirin and NSAIDs unless prescribed
Use small-gauge needles
Avoid contact sports
Protect against falls and injuries
Inform doctors before any procedures
Lifestyle and Dietary Considerations
While diet alone cannot cure thrombocytopenia, it can support recovery:
Foods rich in vitamin B12 and folate
Adequate protein intake
Avoid alcohol
Stay hydrated
Always consult a healthcare provider before using supplements.
Complications of Untreated Thrombocytopenia
Severe blood loss
Intracranial hemorrhage
Organ damage due to internal bleeding
Complications during surgery or childbirth
Early diagnosis and proper management significantly reduce these risks.
When to See a Doctor
Seek medical help if you experience:
Unexplained bruising
Frequent nosebleeds
Heavy menstrual bleeding
Blood in urine or stool
Sudden weakness or dizziness
Frequently Asked Questions (FAQs)
1. Is thrombocytopenia a disease?
No. It is a condition caused by an underlying problem affecting platelet production or survival.
2. Can thrombocytopenia be cured?
Yes, in many cases, especially when the underlying cause is identified and treated.
3. Is thrombocytopenia dangerous?
It can be dangerous if platelet levels drop very low and bleeding occurs.
4. Can thrombocytopenia be temporary?
Yes. Infections, medications, or pregnancy-related cases may be temporary.
5. What platelet count is considered critical?
Counts below 20,000 are considered critical and may cause spontaneous bleeding.
6. Does thrombocytopenia always cause bleeding?
No. Mild cases may not show any symptoms.
7. Can children get thrombocytopenia?
Yes. It can occur in children due to infections, immune conditions, or genetic disorders.
8. Can lifestyle changes improve platelet count?
They help support treatment but do not replace medical care.
9. Is platelet transfusion permanent treatment?
No. It provides temporary relief and is used in emergencies or severe cases.
10. Can thrombocytopenia affect surgery?
Yes. Low platelet counts increase surgical bleeding risk and must be corrected beforehand.
Thrombocytopenia is a common yet potentially serious blood condition that requires careful evaluation and management. While mild cases may go unnoticed, severe thrombocytopenia can lead to dangerous bleeding complications if left untreated.
With proper diagnosis, monitoring, and treatment, most people with thrombocytopenia can lead healthy and normal lives. Awareness of symptoms and early medical consultation play a crucial role in preventing complications.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

Sparsh Doctor List
![]()





