Ischemic colitis is a medical condition in which reduced blood flow to the large intestine (colon) leads to inflammation and tissue injury. It is one of the most common forms of bowel ischemia and can affect individuals of any age, though it is more frequent in older adults. The condition may develop suddenly or gradually and ranges from mild discomfort to a life-threatening emergency if not treated promptly.
This comprehensive guide explains the causes, risk factors, symptoms, diagnostic methods, treatment options, complications, prevention strategies, and when to seek urgent help.
What Is Ischemic Colitis?
Ischemic colitis occurs when the arteries supplying the colon experience reduced blood flow. When blood flow is insufficient, the colon tissues do not receive enough oxygen and nutrients, leading to inflammation, ulceration, and in severe cases, tissue death (necrosis).
The colon is particularly vulnerable because it has “watershed zones”—areas with naturally low blood supply—making them more susceptible during episodes of reduced circulation.
Ischemic colitis is generally categorized into:
Transient ischemic colitis – mild, reversible inflammation
Chronic ischemic colitis – persistent or recurring ischemia leading to long-term changes
Gangrenous ischemic colitis – severe form where tissue death occurs; requires emergency surgery
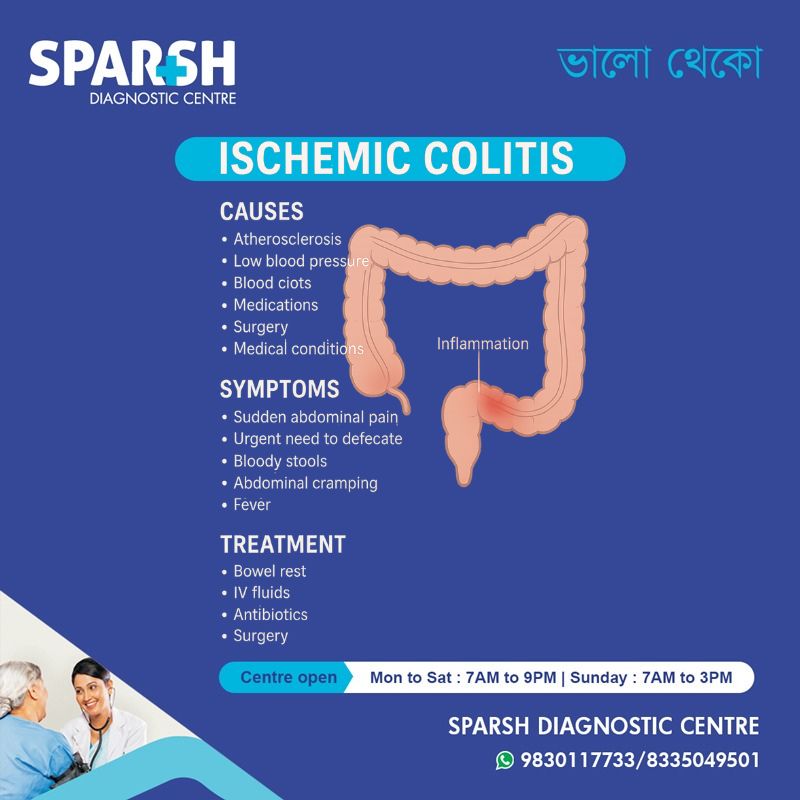
Causes of Ischemic Colitis
Reduced blood flow is the primary cause, but several underlying factors can trigger this decline. Common causes include:
1. Atherosclerosis
Plaque buildup in arteries supplying the colon narrows blood vessels, limiting flow.
2. Low Blood Pressure
Severe dehydration, shock, heart failure, or major surgery can cause sudden drops in blood pressure, reducing intestinal blood flow.
3. Blood Clots
Clots forming in mesenteric arteries can obstruct blood supply abruptly.
4. Medications
Certain drugs may reduce blood flow or constrict vessels:
Hormonal therapies
Diuretics
Vasoconstrictors
Some cardiac medications
5. Surgical or Procedural Factors
Abdominal or vascular surgeries may alter blood supply temporarily.
6. Medical Conditions
Conditions that impair circulation or blood flow include:
Hypercoagulable disorders
Risk Factors
Several factors increase the likelihood of developing ischemic colitis:
Age above 60 years
Surgery involving the aorta or heart
Blood clotting disorders
Use of medications that affect circulation
Symptoms of Ischemic Colitis
Symptoms often develop suddenly, although in some cases they appear gradually.
Common Symptoms Include:
Sudden abdominal pain (usually left-sided)
Urgent need to defecate
Bloody stools or rectal bleeding
Abdominal cramping
Fever (in severe cases)
The severity of symptoms depends on how much of the colon is affected and how long the blood supply remains compromised.
How Is Ischemic Colitis Diagnosed?
Early diagnosis is crucial for preventing complications. A healthcare provider may use the following tests:
1. Medical History & Physical Examination
Assessment of symptoms, risk factors, and abdominal tenderness.
2. Blood Tests
Elevated white blood cell count
Signs of dehydration or metabolic imbalance
3. Stool Tests
To rule out infections such as Clostridium difficile or other pathogens.
4. CT Scan
A CT scan with contrast is the most commonly used imaging test and can show inflammation, thickened bowel walls, and decreased blood flow.
5. Colonoscopy
Provides visual confirmation and may reveal:
Swollen or inflamed areas
Ulcers
Pale or bluish-colored tissue
Biopsies can be taken to confirm ischemia.
6. Doppler Ultrasound or Angiography
Used in complex or severe cases to assess blood vessels supplying the intestines.
Treatment Options for Ischemic Colitis
Treatment depends on the severity and underlying cause.
1. Mild to Moderate Ischemic Colitis
Most patients recover with supportive treatment:
Bowel rest (temporary restriction of oral intake)
IV fluids to restore hydration
Antibiotics to prevent infection
Avoiding medications that reduce blood flow
Symptoms typically improve within 2–3 days.
2. Severe Ischemic Colitis
For extensive tissue damage or persistent symptoms:
Hospitalization
Oxygen therapy
Blood transfusions (if significant bleeding occurs)
Surgery may be required to remove necrotic segments of the colon
3. Surgery
Indicated for:
Perforation
Severe bleeding
Persistent obstruction
Surgery involves removing damaged tissue and restoring healthy bowel continuity.
Possible Complications
While many cases resolve completely, untreated or severe ischemic colitis can lead to:
Colon strictures (narrowing)
Tissue death
Perforation of the colon
Short bowel syndrome (rare)
Prompt treatment significantly reduces the risk of complications.
Prevention Tips
Although not all causes are preventable, lifestyle changes can reduce risk:
Maintain healthy blood pressure
Monitor heart health
Stay hydrated
Manage chronic conditions like diabetes
Manage cholesterol levels
Avoid unnecessary use of vasoconstrictive medications
When to Seek Medical Help
Seek immediate medical attention if you experience:
Sudden severe abdominal pain
Bloody stools
Persistent diarrhea
Fever with abdominal symptoms
Symptoms following major surgery or dehydration
Timely evaluation ensures better outcomes.
FAQ Section
1. Is ischemic colitis life-threatening?
Most cases are mild and resolve with treatment, but severe forms can be life-threatening if not treated promptly.
2. Can ischemic colitis heal on its own?
Mild cases often improve within a few days with supportive care, but medical evaluation is necessary to rule out complications.
3. Is surgery always needed?
No. Surgery is only required in 10–20% of cases where there is gangrene, perforation, or severe complications.
4. Can ischemic colitis recur?
Yes, especially if underlying conditions like heart disease or clotting disorders persist.
5. How long does recovery take?
Most individuals recover within 1–2 weeks, although complete healing of the colon may take longer.
6. What foods should be avoided during recovery?
Limit high-fiber foods, spicy foods, alcohol, and heavy meals until symptoms subside. Gradually reintroduce regular foods as advised.
7. Who is at highest risk?
Older adults, individuals with vascular disease, blood clotting disorders, low blood pressure episodes, and those taking certain medications.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
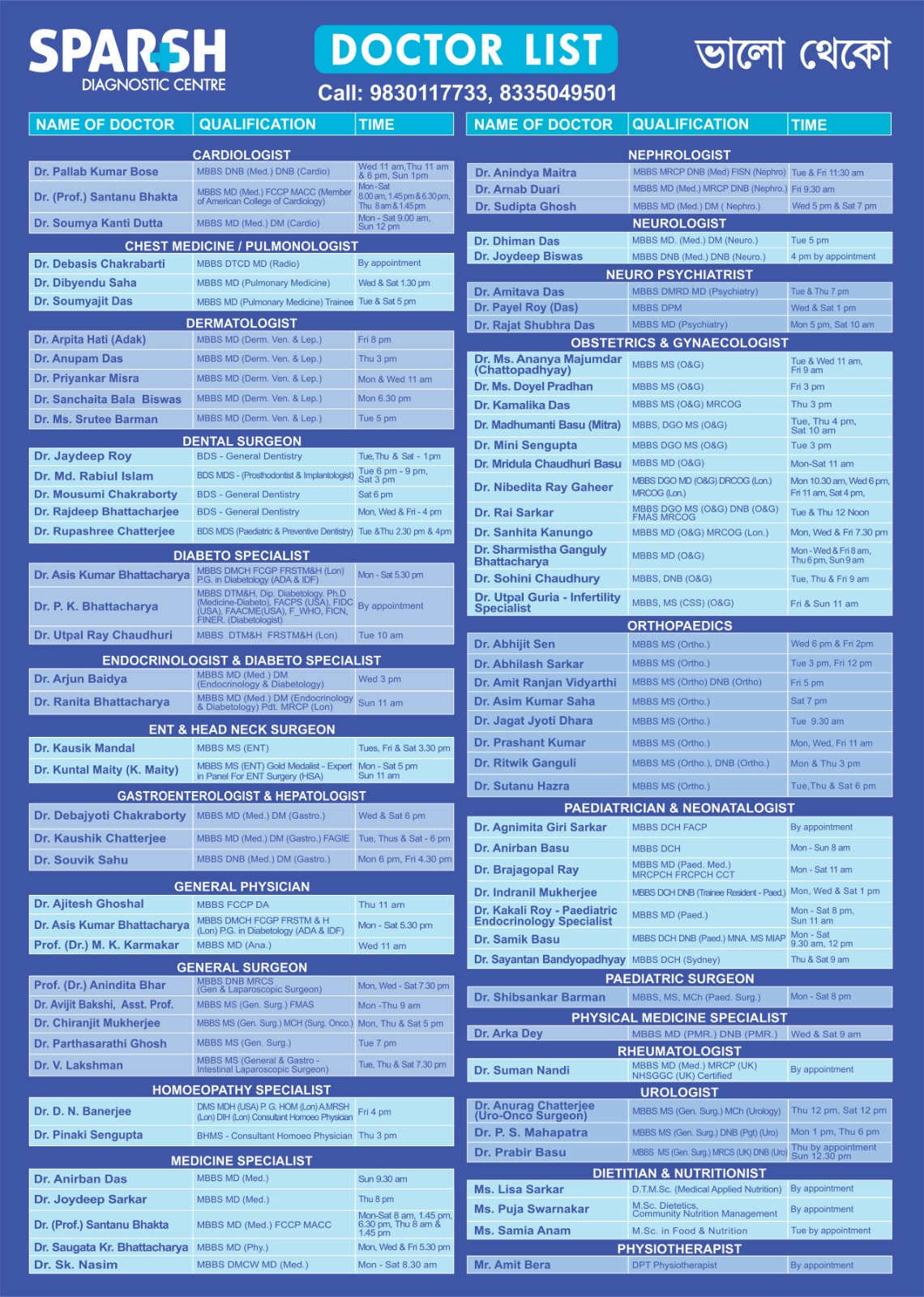
Sparsh Doctor List
![]()





