Hypercoagulable disorders, also known as thrombophilia, are conditions in which the blood has an increased tendency to clot. While blood clotting is a vital process that prevents excessive bleeding, abnormal clot formation can block blood vessels and lead to serious, potentially life-threatening complications. These disorders may be inherited or acquired and often remain undiagnosed until a clotting event occurs.
Understanding hypercoagulable disorders is essential for early detection, effective treatment, and prevention of complications such as deep vein thrombosis, pulmonary embolism, stroke, and recurrent pregnancy loss.
What Are Hypercoagulable Disorders?
Hypercoagulable disorders are conditions that disrupt the body’s natural balance between clot formation and clot breakdown. In healthy individuals, coagulation is carefully regulated by clotting factors and anticoagulant proteins. When this balance is disturbed, the blood may clot too easily or excessively.
These abnormal clots can form in veins or arteries and may partially or completely obstruct blood flow. Some people live with hypercoagulable states for years without symptoms, while others experience recurrent clotting episodes.
Types of Hypercoagulable Disorders
Hypercoagulable disorders are broadly classified into inherited and acquired forms.
Inherited Hypercoagulable Disorders
Inherited thrombophilia results from genetic mutations passed down from one or both parents. Common inherited conditions include:
Factor V Leiden mutation
This is the most common inherited hypercoagulable disorder. It causes resistance to activated protein C, an important anticoagulant, leading to increased clot formation.
Prothrombin gene mutation (G20210A)
This mutation leads to elevated levels of prothrombin, a clotting protein, increasing the risk of thrombosis.
Protein C deficiency
Protein C helps regulate blood clotting. A deficiency results in reduced anticoagulant activity and increased clot risk.
Protein S deficiency
Protein S works alongside protein C. Low levels impair the body’s ability to control clot formation.
Antithrombin III deficiency
Antithrombin inhibits clotting factors. Deficiency leads to uncontrolled clot formation and a higher risk of severe thrombosis.
Acquired Hypercoagulable Disorders
Acquired conditions develop later in life and are often associated with underlying medical conditions or external factors.
Antiphospholipid syndrome (APS)
An autoimmune disorder where antibodies attack phospholipids, increasing the risk of arterial and venous clots and recurrent pregnancy loss.
Cancer-associated thrombosis
Certain cancers and chemotherapy treatments increase clotting risk.
Hormonal factors
Oral contraceptives, hormone replacement therapy, and pregnancy can increase clot formation.
Prolonged immobilization
Extended bed rest, long-distance travel, or paralysis can slow blood flow and promote clot formation.
Chronic inflammatory diseases
Conditions such as inflammatory bowel disease and systemic lupus erythematosus are associated with hypercoagulability.
Causes and Risk Factors
Hypercoagulable disorders develop due to genetic abnormalities, immune system dysfunction, or environmental and lifestyle factors. Common risk factors include:
Previous episodes of deep vein thrombosis or pulmonary embolism
Prolonged immobilization or recent surgery
Pregnancy and the postpartum period
Use of estrogen-containing medications
The presence of multiple risk factors significantly increases the likelihood of clot formation.
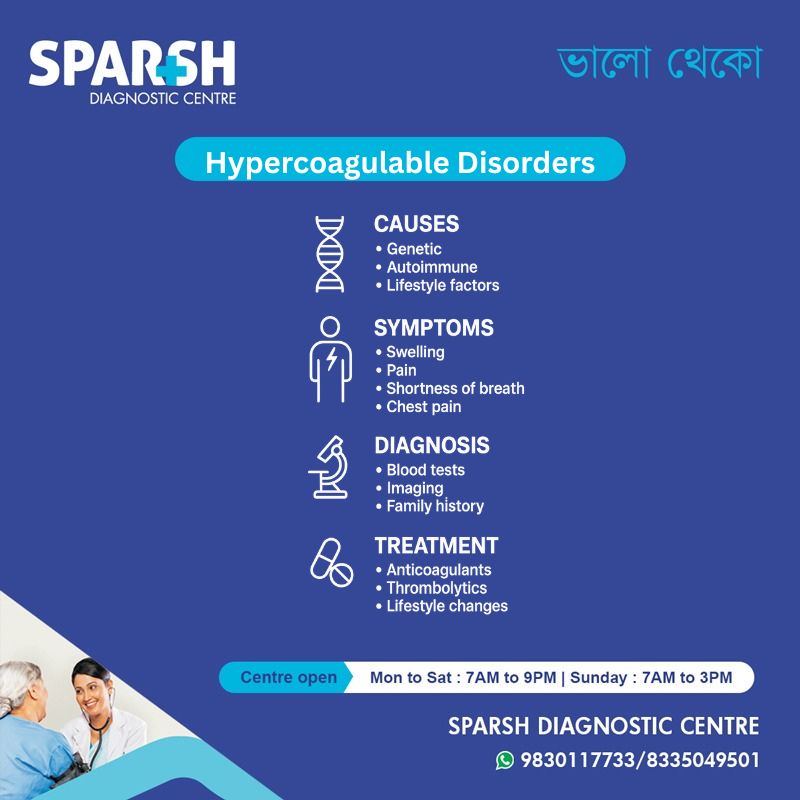
Symptoms of Hypercoagulable Disorders
Many individuals with hypercoagulable disorders remain asymptomatic until a clot develops. Symptoms depend on the location of the clot.
Venous Thrombosis Symptoms
Swelling in one leg or arm
Pain or tenderness, often described as cramping
Warmth and redness over the affected area
Pulmonary Embolism Symptoms
Chest pain that worsens with deep breathing
Coughing, sometimes with blood
Arterial Thrombosis Symptoms
Sudden weakness or numbness
Difficulty speaking or understanding speech
Vision disturbances
Severe headache
Pregnancy-Related Symptoms
Placental insufficiency
Any sudden or unexplained symptoms should be evaluated immediately, as clotting events can progress rapidly.
Complications of Hypercoagulable Disorders
If left untreated, hypercoagulable disorders can lead to serious complications, including:
Recurrent deep vein thrombosis
Stroke or transient ischemic attack
Myocardial infarction
Post-thrombotic syndrome
Pregnancy complications, including fetal loss
Early diagnosis and appropriate management significantly reduce these risks.
Diagnosis of Hypercoagulable Disorders
Diagnosis involves a combination of clinical evaluation, imaging studies, and laboratory tests.
Medical History and Physical Examination
A detailed history helps identify prior clotting events, family history, pregnancy complications, or risk factors such as recent surgery or prolonged immobilization.
Imaging Tests
Doppler ultrasound for suspected deep vein thrombosis
CT pulmonary angiography for pulmonary embolism
Blood Tests
Specialized coagulation tests are used to identify inherited or acquired clotting disorders, including:
Factor V Leiden mutation testing
Prothrombin gene mutation testing
Protein C, protein S, and antithrombin levels
Antiphospholipid antibody panel
Testing is often performed after the acute clotting event has resolved to avoid inaccurate results.
Treatment of Hypercoagulable Disorders
Treatment aims to prevent clot formation, manage existing clots, and reduce the risk of recurrence.
Anticoagulant Medications
Anticoagulants are the mainstay of treatment and may include:
Heparin or low-molecular-weight heparin
Oral anticoagulants such as warfarin
Direct oral anticoagulants (DOACs)
The duration of therapy depends on the underlying disorder, severity, and recurrence risk.
Thrombolytic Therapy
In severe or life-threatening cases, clot-dissolving medications may be used to rapidly restore blood flow.
Lifestyle Modifications
Regular physical activity
Weight management
Adequate hydration
Avoiding prolonged immobility
Pregnancy Management
Women with known hypercoagulable disorders require specialized care during pregnancy, often involving anticoagulation therapy to reduce maternal and fetal risks.
Prevention Strategies
Preventive measures are essential for individuals at high risk of thrombosis. These include:
Prophylactic anticoagulation during surgery or hospitalization
Compression stockings for venous circulation support
Early mobilization after surgery
Regular follow-up and monitoring
Genetic counseling may be beneficial for individuals with inherited hypercoagulable disorders.
Living With a Hypercoagulable Disorder
With appropriate treatment and lifestyle adjustments, most individuals with hypercoagulable disorders can lead normal, active lives. Long-term management often requires collaboration between patients and healthcare providers to ensure medication adherence, monitor for side effects, and promptly address new symptoms.
Patient education plays a vital role in recognizing early warning signs of clot formation and seeking timely medical care.
Frequently Asked Questions (FAQ)
What is the most common hypercoagulable disorder?
Factor V Leiden mutation is the most common inherited hypercoagulable disorder, particularly in people of European descent.
Can hypercoagulable disorders be cured?
Most hypercoagulable disorders cannot be cured, but they can be effectively managed with anticoagulation therapy and lifestyle modifications.
Who should be tested for hypercoagulable disorders?
Testing is recommended for individuals with unexplained or recurrent blood clots, clots at a young age, a strong family history, or recurrent pregnancy loss.
Are hypercoagulable disorders hereditary?
Some forms are inherited, while others are acquired due to autoimmune conditions, cancer, medications, or lifestyle factors.
Is long-term anticoagulation always necessary?
Not always. The duration of anticoagulation depends on the underlying cause, severity of the disorder, and risk of recurrence.
Can pregnancy trigger hypercoagulable disorders?
Pregnancy itself increases clotting risk and may unmask an underlying hypercoagulable disorder.
What lifestyle changes help reduce clot risk?
Staying active, maintaining a healthy weight, avoiding smoking, staying hydrated, and minimizing prolonged immobility can reduce clot risk.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

Sparsh Doctor List
![]()






[…] Hypercoagulable disorders […]