The human body is a complex system that functions smoothly thanks to the autonomic nervous system (ANS). This system controls automatic body functions such as heart rate, blood pressure, digestion, body temperature, and breathing. When the ANS does not function properly, the condition is known as dysautonomia.
Dysautonomia is not a single disorder but rather an umbrella term used to describe a group of medical conditions caused by a malfunction of the autonomic nervous system. These disorders can range from mild to severe and, in some cases, may significantly affect daily life.
This blog provides a detailed understanding of dysautonomia, including its types, causes, symptoms, diagnosis, treatment options, and management strategies.
What is Dysautonomia?
Dysautonomia refers to a dysfunction of the autonomic nervous system (ANS), which regulates involuntary body processes. Since the ANS influences vital functions like blood circulation, digestion, and breathing, dysfunction can lead to widespread health issues.
There are many different types of dysautonomia, and they can be primary (occurring on their own) or secondary (caused by another condition).
Types of Dysautonomia
Postural Orthostatic Tachycardia Syndrome (POTS):
Characterized by an abnormally high heart rate upon standing.
Common in younger individuals, particularly women.
Neurocardiogenic Syncope (NCS):
The most common form, causing fainting due to a sudden drop in heart rate and blood pressure.
Multiple System Atrophy (MSA):
A rare, progressive neurological disorder that affects multiple systems in the body.
Causes a gradual failure of the autonomic nervous system without other neurological involvement.
A rare genetic condition affecting the development and function of autonomic and sensory nerves.
Secondary Dysautonomia:
Results from other medical conditions such as diabetes, Parkinson’s disease, autoimmune disorders, or chronic illnesses.
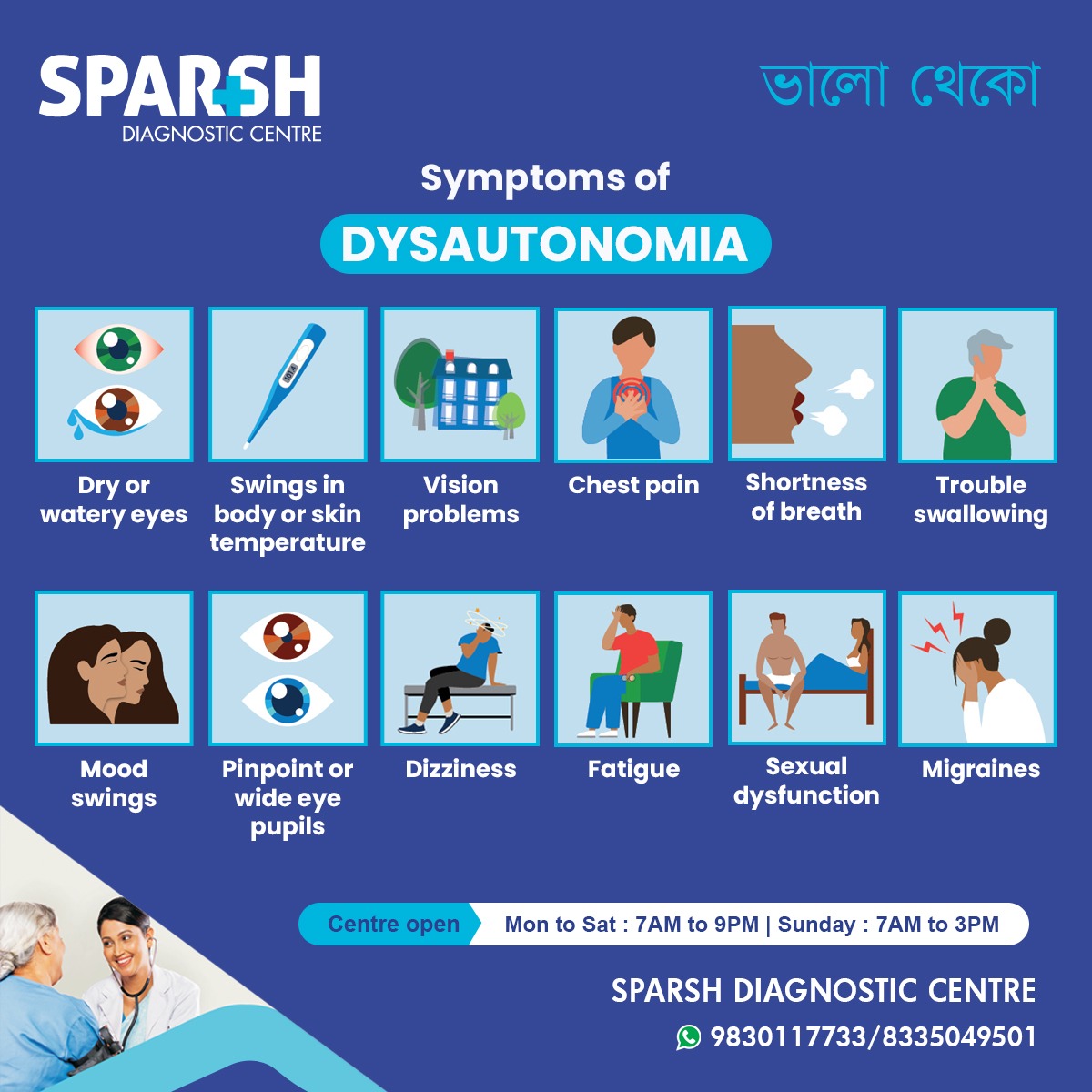
Symptoms of Dysautonomia
The symptoms can vary depending on the type and severity of the condition. According to Sparsh Diagnostic Centre’s awareness material, common symptoms include:
Dry or watery eyes
Swings in body or skin temperature
Vision problems
Mood swings
Pinpoint or wide pupils
Dizziness or fainting spells
Sexual dysfunction
Other possible symptoms include:
Digestive issues (constipation, bloating, nausea)
Difficulty regulating body temperature
Brain fog or trouble concentrating
These symptoms often worsen when standing up or after exertion, making everyday activities challenging.
Causes and Risk Factors
Dysautonomia can develop due to a variety of underlying causes:
Genetic Factors – Some forms, such as familial dysautonomia, are inherited.
Autoimmune Disorders – Conditions like lupus, multiple sclerosis, or Sjögren’s syndrome may trigger autonomic dysfunction.
Chronic Diseases – Diabetes, Parkinson’s disease, and amyloidosis are linked to dysautonomia.
Infections – Viral or bacterial infections may damage autonomic nerve fibers.
Physical Trauma – Head injuries or nerve damage may affect ANS functioning.
Neurodegenerative Diseases – Progressive conditions such as MSA can cause dysautonomia.
Risk factors include family history, long-term diabetes, autoimmune conditions, and chronic infections.
Diagnosis of Dysautonomia
Diagnosing dysautonomia can be complex due to overlapping symptoms. A healthcare provider may use a combination of tests, including:
Tilt Table Test: Measures how blood pressure and heart rate respond to changes in posture.
Autonomic Reflex Testing: Evaluates the functioning of the autonomic nervous system.
Heart Rate Variability Tests: Detects abnormal heart responses.
QSART (Quantitative Sudomotor Axon Reflex Test): Assesses sweating response.
Blood Tests: To rule out other conditions.
Imaging Tests (MRI/CT): To check for neurological or structural issues.
Since dysautonomia symptoms can mimic other disorders, a proper diagnosis requires thorough evaluation by a neurologist or cardiologist.
Treatment of Dysautonomia
There is no universal cure for dysautonomia, but treatment aims to manage symptoms, improve quality of life, and address underlying causes.
1. Lifestyle Modifications
Increasing fluid and salt intake to maintain blood pressure.
Wearing compression stockings to improve circulation.
Avoiding prolonged standing and hot environments.
Elevating the head of the bed to reduce symptoms.
2. Medications
Fludrocortisone to increase blood volume.
Midodrine to raise blood pressure.
Beta-blockers to manage heart rate.
SSRIs/SNRIs for regulating autonomic responses.
Pain medications for associated discomfort.
3. Physical Therapy
Light exercises to improve circulation.
Strengthening core muscles to support blood flow.
Graded exercise therapy for POTS patients.
4. Dietary Adjustments
Frequent small meals instead of large ones.
Balanced diet rich in vitamins and minerals.
Limiting alcohol and caffeine.
5. Psychological Support
Counseling or therapy to manage mood swings, anxiety, or depression linked with dysautonomia.
Living with Dysautonomia
Managing dysautonomia requires a holistic approach. Many patients benefit from:
Support groups and counseling.
Monitoring symptoms with wearable devices.
Regular follow-ups with healthcare providers.
Adaptive strategies like using mobility aids when needed.
With the right care, patients can significantly improve their quality of life, even though flare-ups may still occur.
Complications of Dysautonomia
If left unmanaged, dysautonomia may lead to:
Frequent fainting and falls
Reduced ability to work or perform daily tasks
Severe fatigue and disability
Increased risk of cardiovascular problems
Emotional and psychological stress
Prevention and Outlook
While not all cases can be prevented, some lifestyle changes and timely management can reduce severity:
Managing underlying conditions like diabetes.
Avoiding triggers such as dehydration, heat, and stress.
Early diagnosis and treatment for better prognosis.
The outlook depends on the type of dysautonomia. Some forms are manageable with treatment, while progressive forms like MSA may worsen over time.
FAQs on Dysautonomia
1. What is the most common type of dysautonomia?
The most common type is neurocardiogenic syncope (NCS), which causes fainting due to abnormal blood pressure and heart rate regulation.
2. Can dysautonomia be cured?
Currently, there is no permanent cure. However, treatment can effectively control symptoms and improve quality of life.
3. Is dysautonomia a life-threatening condition?
Most forms are not life-threatening, but severe cases such as multiple system atrophy can significantly impact life expectancy.
4. What foods help with dysautonomia?
A diet rich in fluids, salt, lean proteins, whole grains, and electrolytes can help maintain stability. Avoiding alcohol and large meals may reduce symptoms.
5. Who is at risk of developing dysautonomia?
Individuals with autoimmune conditions, diabetes, Parkinson’s disease, or a family history of autonomic disorders are at higher risk.
6. Can exercise help with dysautonomia?
Yes, gentle exercises like swimming, yoga, and recumbent biking can improve blood circulation and reduce symptoms. Always consult a doctor before starting.
7. How is dysautonomia different from chronic fatigue syndrome?
While both cause fatigue, dysautonomia specifically involves dysfunction of the autonomic nervous system, whereas chronic fatigue syndrome has broader causes.
Dysautonomia is a complex and often misunderstood disorder that affects millions of people worldwide. By recognizing symptoms such as dizziness, fatigue, chest pain, vision problems, and mood swings, individuals can seek timely medical evaluation. Although there is no cure, a combination of lifestyle modifications, medical treatment, and psychological support can significantly improve daily living.
If you or a loved one experience persistent symptoms of dysautonomia, consult a healthcare provider for a thorough diagnosis and treatment plan.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()





[…] known as idiopathic orthostatic hypotension, PAF is now recognized as a form of dysautonomia—a group of conditions in which the autonomic nervous system does not work properly. It primarily […]
[…] help determine if dysautonomia is contributing to postprandial […]