Tuberculosis (TB) is most commonly associated with the lungs, but it can also affect other parts of the body—a form known as extrapulmonary TB. One such serious manifestation is abdominal tuberculosis, which primarily impacts the gastrointestinal tract, peritoneum, lymph nodes, or solid abdominal organs like the liver and spleen.
Despite its rarity compared to pulmonary TB, abdominal tuberculosis can be life-threatening if left undiagnosed or untreated. Early identification of symptoms and accurate testing are essential to preventing complications such as intestinal obstruction or ascites. This blog offers a comprehensive guide to abdominal tuberculosis, covering everything from symptoms and causes to diagnosis and treatment.
What is Abdominal Tuberculosis?
Abdominal tuberculosis is a type of extrapulmonary tuberculosis that involves the gastrointestinal system, peritoneum, abdominal lymph nodes, or solid organs. It is caused by Mycobacterium tuberculosis, the same bacterium that causes pulmonary TB.
Forms of Abdominal TB:
Gastrointestinal TB – affects the intestines, especially the ileocecal region.
Peritoneal TB – involves the peritoneum and may lead to ascites (fluid accumulation).
Lymph node TB – targets abdominal lymph nodes.
Solid organ TB – can affect liver, spleen, or pancreas in rare cases.
Causes and Risk Factors
Abdominal TB usually spreads through:
Hematogenous spread from active pulmonary tuberculosis.
Swallowing infected sputum from pulmonary TB patients.
Contaminated food or milk (especially unpasteurized dairy).
Lymphatic spread from infected mesenteric lymph nodes.
Risk Factors:
Poor hygiene and sanitation
Living in overcrowded conditions
History of TB or close contact with TB patients
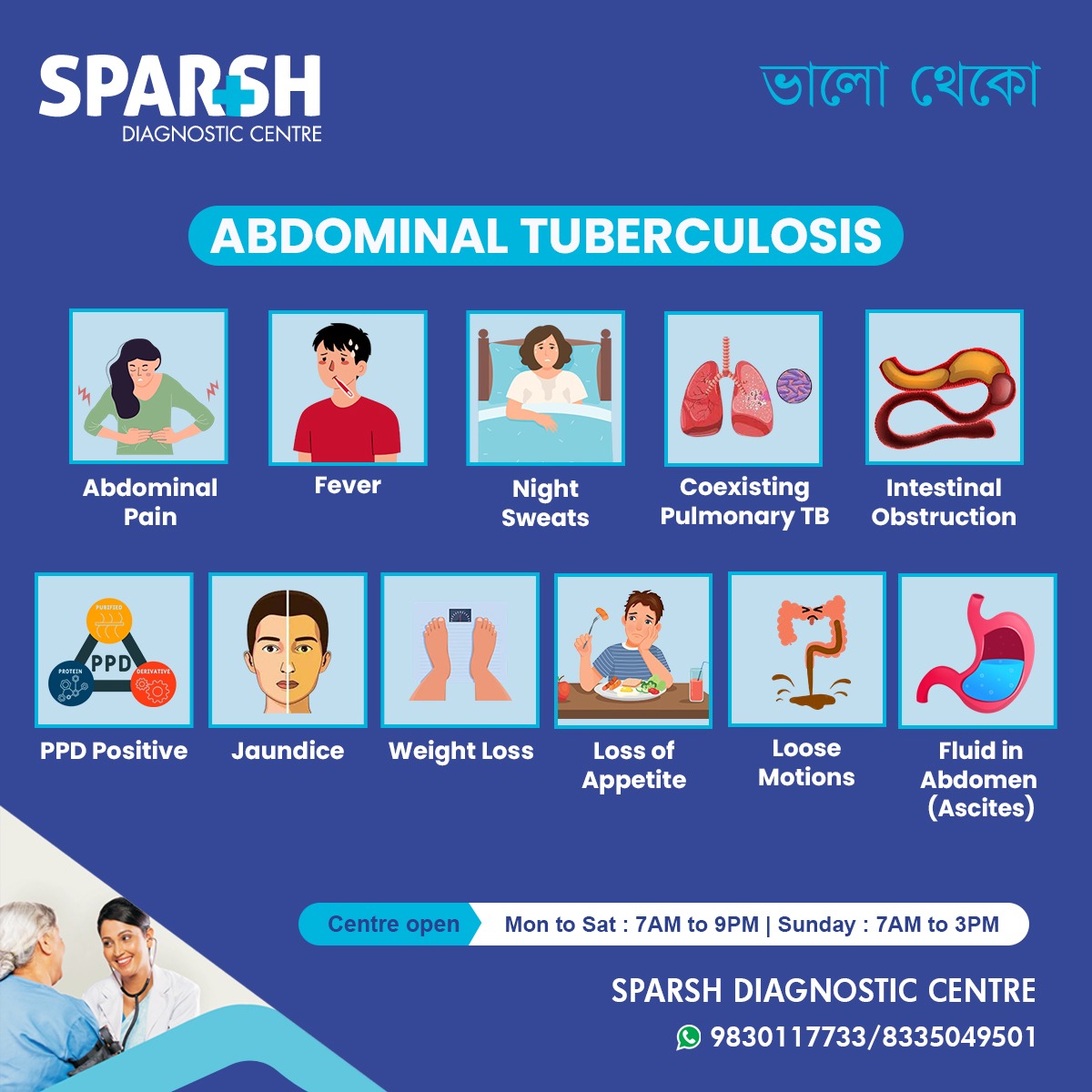
Symptoms of Abdominal Tuberculosis
Abdominal TB can mimic various gastrointestinal disorders, making it hard to diagnose without proper testing. Common signs and symptoms include:
1. Abdominal Pain
Usually persistent and dull, especially in the lower right quadrant.
2. Fever
Low-grade, often accompanied by chills and fatigue.
3. Night Sweats
Profuse sweating during sleep, a hallmark of tuberculosis.
4. Weight Loss
Unexplained, rapid weight loss despite normal or decreased appetite.
5. Loss of Appetite
A general disinterest in food, contributing to malnutrition.
6. Loose Motions
Chronic diarrhea may occur in some patients.
7. Jaundice
Seen when the liver is involved, leading to yellowing of the skin and eyes.
8. Fluid in the Abdomen (Ascites)
Swelling and fluid buildup in the abdomen due to peritoneal TB.
9. Coexisting Pulmonary TB
Many patients also have TB in their lungs, detectable via chest X-rays or sputum tests.
10. Positive PPD (Mantoux Test)
Indicates prior exposure to TB bacteria.
11. Intestinal Obstruction
Due to strictures, adhesions, or mass formation in the intestines.
How is Abdominal Tuberculosis Diagnosed?
Due to the nonspecific symptoms, a combination of diagnostic tools is often needed:
1. Blood Tests
ESR (Elevated)
CBC (Anemia common)
TB Gold or Mantoux test (for TB exposure)
2. Imaging Tests
Ultrasound – detects ascites, thickened bowel loops, lymphadenopathy.
CT Scan – more detailed evaluation of abdominal organs.
X-ray – to check for coexisting pulmonary TB.
3. Ascitic Fluid Analysis
High protein content
Lymphocytic predominance
ADA (adenosine deaminase) levels > 40 U/L strongly suggest TB.
4. Endoscopy/Colonoscopy
Allows visual examination and biopsy of affected intestinal mucosa.
5. Laparoscopy
For direct inspection and biopsy of peritoneal lesions.
6. Histopathological Examination
Granulomatous inflammation with caseation confirms TB.
Differential Diagnoses
Due to its vague symptoms, abdominal TB is often misdiagnosed as:
Abdominal cancers
Intestinal obstruction
Ovarian malignancies (in females with ascites)
Hence, a multidisciplinary diagnostic approach is crucial.
Treatment of Abdominal Tuberculosis
The mainstay of treatment is anti-tuberculosis therapy (ATT).
Standard Regimen (as per WHO guidelines):
Intensive Phase (2 months):
Isoniazid (H)
Rifampicin (R)
Pyrazinamide (Z)
Ethambutol (E)
Continuation Phase (4–7 months):
Isoniazid (H)
Rifampicin (R)
Total Duration: Usually 6–9 months, but extended up to 12 months in complicated cases.
Supportive Treatments:
Nutritional support and supplements
Pain management
Laxatives for constipation
Diuretics if ascites is present
Surgery:
Required in complicated cases like:
Intestinal perforation
Strictures causing obstruction
Persistent ascites not responding to drugs
Prognosis and Recovery
With timely diagnosis and full adherence to treatment, the prognosis of abdominal TB is excellent. However, delays can lead to complications such as:
Bowel obstruction
Intestinal perforation
Relapse can occur if the treatment course is not completed.
Prevention of Abdominal Tuberculosis
While there’s no foolproof way to prevent TB entirely, several strategies can lower the risk:
1. BCG Vaccination
Administered in infancy to protect against severe forms of TB.
2. Avoid Contaminated Food
Ensure milk is pasteurized and water is safe for consumption.
3. Timely Treatment of Pulmonary TB
Reduces the risk of extrapulmonary spread.
4. Hygiene and Sanitation
Especially in densely populated or resource-poor settings.
5. Regular Health Check-Ups
Especially if exposed to TB or living in high-risk areas.
When Should You See a Doctor?
You should seek immediate medical attention if you experience:
Night sweats and fatigue
At Sparsh Diagnostic Centre, we offer comprehensive diagnostic services tailored to detect complex conditions like abdominal tuberculosis. With our advanced imaging technologies, expert radiologists, and accurate lab testing, we ensure timely and precise diagnosis.
Our key services include:
TB Gold Testing and PPD
Biopsy and Histopathology
Routine blood work and liver function tests
Specialist consultations
We are open from 7 AM to 9 PM (Monday to Saturday) and 7 AM to 3 PM on Sundays, making healthcare accessible and convenient for all.
Abdominal tuberculosis is a serious, but treatable, condition. What makes it challenging is its ability to mimic other diseases. Awareness of its symptoms and timely diagnosis can make a life-changing difference.
If you or someone you know is experiencing unexplained abdominal symptoms, don’t ignore the signs. Reach out to a trusted healthcare provider for thorough evaluation and care.
FAQs on Abdominal Tuberculosis
Q1. Is abdominal tuberculosis contagious?
A: Not directly. It usually arises as a complication of pulmonary TB, which is contagious through respiratory droplets.
Q2. Can abdominal TB return after treatment?
A: If treatment is incomplete or the immune system is weak, relapse is possible. Adherence to the full course is vital.
Q3. Is surgery always necessary for abdominal TB?
A: No. Most cases respond well to medication, but surgery is needed in some complicated cases.
Q4. What is the role of diet during treatment?
A: A protein-rich, balanced diet helps in faster recovery and combats malnutrition.
Contact Us
📍 Sparsh Diagnostic Centre
📞 9830117733 / 8335049501
🌐 www.sparshdiagnostica.com
Stay informed. Stay healthy.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()





