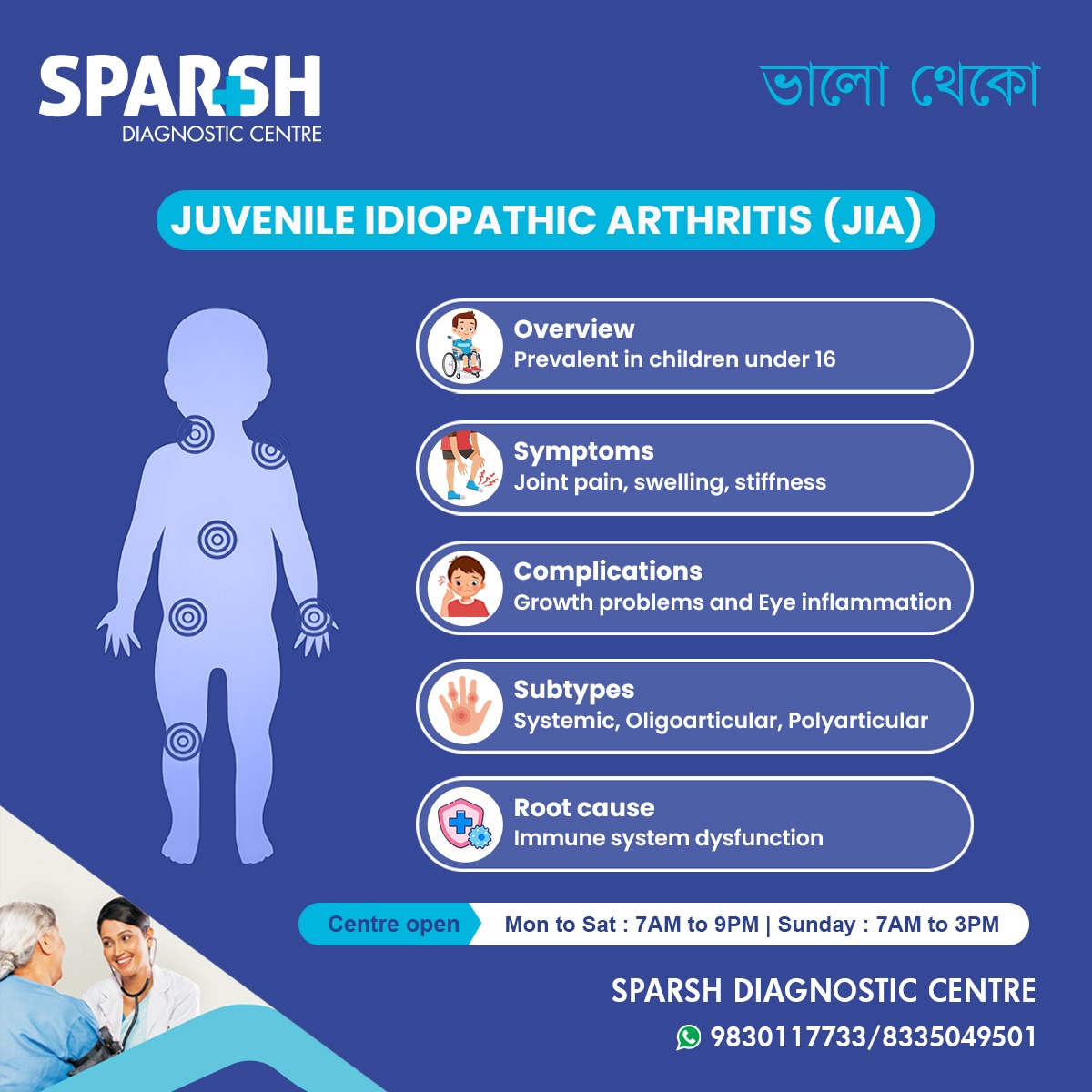
Juvenile Idiopathic Arthritis (JIA) is the most common type of arthritis in children and adolescents. It’s a chronic autoimmune condition that can significantly impact a child’s quality of life if left untreated. This comprehensive guide explores the causes, symptoms, subtypes, diagnosis, treatment, and long-term management of JIA—empowering parents and caregivers with the knowledge they need to support affected children.
What Is Juvenile Idiopathic Arthritis?
Juvenile Idiopathic Arthritis (JIA) refers to a group of autoimmune disorders that cause persistent joint inflammation in children under the age of 16. The term “idiopathic” means the exact cause is unknown. JIA is not a single disease but a category encompassing several subtypes, each with distinct characteristics.
- Autoimmune nature: The immune system mistakenly attacks healthy joint tissues.
- Chronic condition: Symptoms can persist for months, years, or even a lifetime.
- Not contagious: JIA is not caused by infection and cannot be spread from child to child.
Causes and Risk Factors
While the exact cause of JIA remains unknown, researchers believe a combination of genetic predisposition and environmental triggers may play a role.
- Genetics: Certain genes may increase susceptibility.
- Immune dysfunction: The immune system attacks the synovium (joint lining).
- Environmental factors: Viral infections or stress may trigger onset in genetically predisposed children.
Common Symptoms of JIA
Symptoms vary depending on the subtype but generally include:
- Joint pain and stiffness, especially in the morning
- Swelling and warmth in affected joints
- Fatigue and irritability
- Fever and rash (in systemic JIA)
- Eye inflammation (uveitis), which may lead to vision problems
- Growth disturbances due to chronic inflammation
Types of Juvenile Idiopathic Arthritis
JIA is classified into several subtypes based on symptoms, number of joints affected, and presence of systemic features:
| Subtype | Description |
|---|---|
| Oligoarticular JIA | Affects 4 or fewer joints; most common form; often involves knees or ankles |
| Polyarticular JIA | Affects 5 or more joints; symmetrical involvement; resembles adult rheumatoid arthritis |
| Systemic JIA | Includes fever, rash, and organ inflammation; affects entire body |
| Enthesitis-related JIA | Involves inflammation at tendon attachment sites; common in boys over 8 |
| Psoriatic JIA | Associated with psoriasis; may involve fingers and toes |
| Undifferentiated JIA | Doesn’t fit into other categories or overlaps multiple types |
Diagnosis and Testing
Diagnosing JIA involves ruling out other conditions and confirming persistent joint inflammation.
- Physical examination: Assess joint swelling, range of motion, and systemic symptoms.
- Blood tests: ESR, CRP, ANA, RF to detect inflammation and autoantibodies.
- Imaging: X-rays, MRI, or ultrasound to evaluate joint damage.
- Eye exams: Regular screening for uveitis.
Early diagnosis is crucial to prevent long-term joint damage and complications.
Treatment Options
Treatment aims to reduce inflammation, relieve symptoms, and prevent joint damage.
1. Medications
- NSAIDs: Ibuprofen or naproxen for pain and inflammation.
- DMARDs: Methotrexate is commonly used to slow disease progression.
- Biologics: TNF inhibitors (e.g., etanercept) for severe or resistant cases.
- Corticosteroids: Used sparingly for flare-ups or systemic symptoms.
2. Physical Therapy
- Improves joint mobility and muscle strength.
- Prevents contractures and deformities.
3. Occupational Therapy
- Helps children adapt daily activities to maintain independence.
4. Eye Care
- Regular monitoring and treatment for uveitis.
5. Psychosocial Support
- Counseling and support groups for emotional well-being.
Long-Term Outlook and Management
With early intervention and consistent treatment, many children with JIA lead active, fulfilling lives.
- Remission is possible in some cases.
- Regular follow-ups are essential to monitor disease activity.
- Lifestyle adjustments like balanced nutrition, exercise, and stress management support overall health.
Living with JIA: Tips for Parents
- Educate yourself about the condition and treatment options.
- Communicate with teachers to accommodate physical limitations.
- Encourage gentle exercise like swimming or yoga.
- Monitor medication side effects and report concerns to your doctor.
- Support emotional health through open conversations and peer support.
Frequently Asked Questions (FAQs)
Q1: Is JIA curable?
While there is no permanent cure, many children achieve remission with proper treatment.
Q2: Can JIA affect organs other than joints?
Yes. Systemic JIA can affect the heart, liver, and lymph nodes. Uveitis can impact the eyes.
Q3: Is JIA hereditary?
Genetics may play a role, but JIA is not directly inherited like some genetic disorders.
Q4: Can children with JIA play sports?
Yes, with guidance from healthcare providers. Low-impact activities are encouraged.
Q5: How often should children with JIA see a doctor?
Regular check-ups every 3–6 months, or as advised by the rheumatologist.
Juvenile Idiopathic Arthritis is a complex condition, but with early diagnosis, personalized treatment, and strong support systems, children can thrive. Awareness and education are key to improving outcomes and reducing stigma around pediatric autoimmune diseases.
If you suspect your child may have symptoms of JIA, consult a pediatric rheumatologist promptly. For diagnostic services and compassionate care, visit Sparsh Diagnostic Centre—open daily with expert clinicians ready to help.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()




[…] 6. Juvenile Idiopathic Arthritis (JIA) […]
[…] Juvenile idiopathic arthritis (JIA) […]