Contaminated water can be the source of serious health issues. Waterborne diseases are illnesses caused by consuming or coming into contact with contaminated water. They are among the leading causes of morbidity and mortality worldwide, particularly in developing countries where access to clean and safe drinking water is limited.
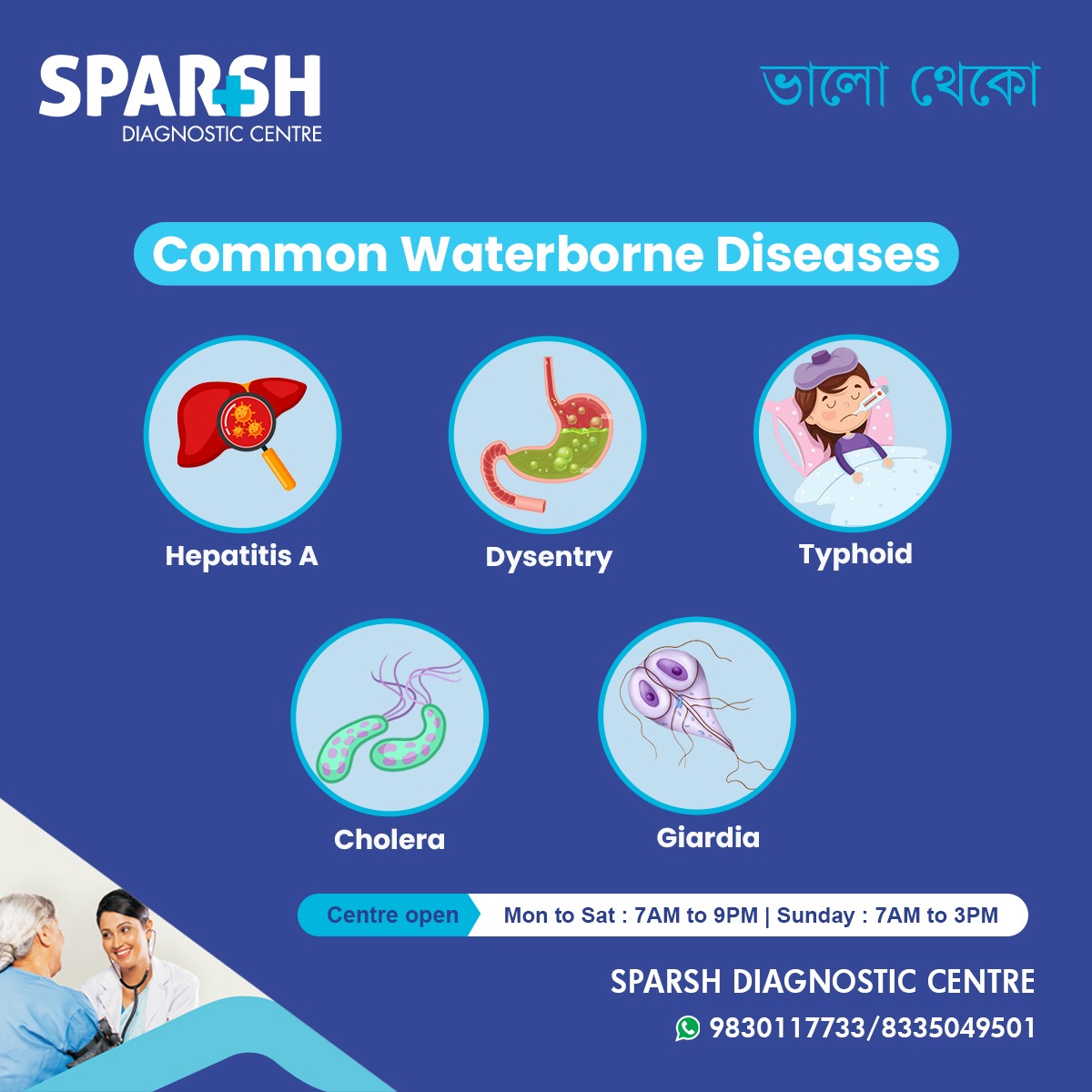
Every year, millions of people suffer from diseases like Hepatitis A, Dysentery, Typhoid, Cholera, and Giardiasis—all of which are transmitted through unsafe water. Understanding these diseases, their symptoms, and preventive measures is essential for maintaining public health.
In this blog, we will cover:
What waterborne diseases are
Causes and modes of transmission
Symptoms of common waterborne diseases
Treatment options
Prevention strategies
Frequently asked questions
What Are Waterborne Diseases?
Waterborne diseases are infections caused by microorganisms such as bacteria, viruses, and parasites that contaminate water sources. These pathogens typically enter the body through drinking, bathing, cooking, or washing food with unsafe water. Poor sanitation, open defecation, and inadequate waste management increase the risk of contamination.
Globally, waterborne diseases are a major public health concern. According to the World Health Organization (WHO), unsafe water, poor sanitation, and inadequate hygiene account for around 505,000 deaths annually due to diarrheal diseases.
Causes of Waterborne Diseases
The main causes include:
Contaminated Drinking Water – Presence of pathogens like E. coli, Vibrio cholerae, Salmonella typhi, and parasites such as Giardia lamblia.
Poor Sanitation – Open defecation and poor sewage systems contaminate rivers, lakes, and groundwater.
Flooding During Monsoons – Heavy rains often mix sewage with drinking water sources, increasing contamination risks.
Lack of Hygiene – Improper handwashing or food handling can spread infection.
Unsafe Storage – Even clean water can become contaminated if stored in unclean containers.
Common Waterborne Diseases and Their Symptoms
Let’s explore the most common waterborne diseases and how they affect human health:
1. Hepatitis A
Hepatitis A is a viral infection that affects the liver. It spreads when people consume food or water contaminated with the Hepatitis A virus (HAV).
Symptoms include:
While Hepatitis A usually resolves on its own, in some cases, it can cause severe liver damage. Vaccination is an effective preventive measure.
2. Dysentery
Dysentery is an infection of the intestines caused by bacteria (Shigella) or amoebas (Entamoeba histolytica). It is often spread through contaminated water or food.
Symptoms include:
Severe diarrhea with blood or mucus
Abdominal cramps
Nausea and vomiting
If untreated, dysentery can lead to severe dehydration, especially in children and elderly individuals.
3. Typhoid Fever
Typhoid fever is caused by the bacterium Salmonella typhi. It spreads through contaminated water, poor sanitation, and unhygienic food practices.
Symptoms include:
High fever (often prolonged)
Weakness and fatigue
Abdominal pain
Constipation or diarrhea
Typhoid can become life-threatening if left untreated, as it may cause intestinal perforation or bleeding. Vaccination and antibiotics are essential preventive and treatment measures.
4. Cholera
Cholera is one of the most severe waterborne diseases, caused by the bacterium Vibrio cholerae. It spreads rapidly in areas with poor sanitation and contaminated drinking water.
Symptoms include:
Profuse watery diarrhea (“rice-water stools”)
Severe dehydration
Rapid heart rate
Muscle cramps
Cholera outbreaks can spread quickly and cause deaths within hours if patients are not given immediate rehydration therapy.
5. Giardiasis (Giardia Infection)
Giardiasis is caused by the parasite Giardia lamblia. It spreads through contaminated drinking water and sometimes through person-to-person contact.
Symptoms include:
Diarrhea (often greasy and foul-smelling)
Abdominal cramps
Fatigue
Nausea
Although rarely fatal, giardiasis can lead to malnutrition and chronic digestive issues if untreated.
Diagnosis of Waterborne Diseases
Accurate diagnosis is critical for timely treatment. Some common diagnostic methods include:
Stool Tests – Detect parasites, bacteria, or blood.
Blood Tests – Identify antibodies or antigens for specific infections like typhoid and hepatitis A.
Rapid Diagnostic Tests – Quick identification of pathogens like cholera.
Ultrasound/Imaging – Sometimes used in severe cases of hepatitis or intestinal complications.
Treatment of Common Waterborne Diseases
Treatment depends on the specific infection but generally involves:
Rehydration Therapy – To replace lost fluids and electrolytes, especially in cholera and dysentery.
Antibiotics/Antivirals – Prescribed for bacterial infections like typhoid, cholera, and dysentery.
Antiparasitic Drugs – For infections like giardiasis and amoebic dysentery.
Rest and Nutrition – Adequate rest, a balanced diet, and supportive care help recovery.
Hospitalization – Severe cases with complications like dehydration or organ failure may require hospitalization.
Prevention of Waterborne Diseases
“Prevention is better than cure” holds true for waterborne illnesses. Key preventive measures include:
Individual and Household Practices
Always boil, filter, or purify drinking water.
Wash hands with soap before eating and after using the toilet.
Store water in clean, covered containers.
Wash fruits and vegetables thoroughly.
Avoid consuming street food during monsoons.
Community-Level Practices
Improve sanitation and sewage systems.
Regular chlorination of public water supplies.
Health awareness campaigns about safe water practices.
Encourage vaccinations for Hepatitis A and Typhoid.
Global and Local Burden
Waterborne diseases remain a pressing health issue, especially in India and other tropical countries where monsoon flooding and poor sanitation are common. Rural and slum areas are particularly vulnerable.
According to the UNICEF report, diarrheal diseases remain a leading killer of children under five, accounting for more than 1,200 child deaths per day worldwide. Strengthening water, sanitation, and hygiene (WASH) initiatives can significantly reduce these numbers.
When to See a Doctor?
Seek medical help if you experience:
Persistent high fever
Severe dehydration (dry mouth, low urine output, dizziness)
Jaundice
Severe abdominal pain
Timely diagnosis and treatment can prevent complications and save lives.
Waterborne diseases such as Hepatitis A, Dysentery, Typhoid, Cholera, and Giardiasis are preventable yet remain a significant threat to global health. Access to safe drinking water, improved sanitation, and personal hygiene are the cornerstones of prevention.
At Sparsh Diagnostic Centre, we provide accurate diagnostic tests to detect infections early, ensuring timely treatment and recovery. Remember, clean water is not just a necessity—it’s a right. Protect yourself and your family by staying informed and practicing safe water habits.
FAQs on Common Waterborne Diseases
1. What are the most common waterborne diseases?
The most common waterborne diseases include Hepatitis A, Dysentery, Typhoid, Cholera, and Giardiasis.
2. How do waterborne diseases spread?
They spread through consumption of contaminated water, poor sanitation, unhygienic food practices, and flooding during monsoons.
3. Can waterborne diseases be fatal?
Yes. Diseases like cholera and typhoid can become life-threatening if not treated promptly.
4. How can I protect my family from waterborne diseases?
Drink boiled/filtered water, maintain hygiene, wash hands regularly, and get vaccinated against diseases like Hepatitis A and Typhoid.
5. When should I see a doctor for waterborne disease symptoms?
If you have severe diarrhea, prolonged fever, blood in stool, dehydration, or jaundice, seek medical help immediately.
6. Can children get vaccinated for waterborne diseases?
Yes. Vaccines are available for Hepatitis A and Typhoid and are recommended for children in high-risk areas.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()