Anaphylaxis is one of the most serious emergencies related to allergies. It can come on fast, affect several parts of the body at once, and become life-threatening within minutes if it isn’t treated right away. While most people think of allergies as mild issues like sneezing, itching, or a rash, anaphylaxis sits at the most dangerous end of the spectrum.
In this guide, we’ll walk through what anaphylaxis really is, why it happens, what it looks like, how it’s treated in an emergency, who is at higher risk, and how to prevent it from happening again.
What Is Anaphylaxis?
Anaphylaxis is a severe allergic reaction that spreads throughout the body. It usually happens after someone who is already allergic to a substance is exposed to it again.
In simple terms, the immune system overreacts. It treats a normally harmless substance—like peanuts or bee venom—as a major threat. That reaction triggers the sudden release of powerful chemicals such as histamine. These chemicals quickly affect the skin, lungs, heart, blood vessels, and digestive system.
Without prompt treatment—especially with epinephrine—the reaction can escalate to dangerously low blood pressure, blocked airways, cardiac arrest, and even death.
Why Does Anaphylaxis Escalate So Quickly?
To understand the speed and severity of anaphylaxis, it helps to know what’s happening inside the body.
The First Exposure: Sensitization
At some point, the immune system misidentifies a substance (for example, peanuts or insect venom) as harmful. It creates specific antibodies called IgE to “remember” that substance.
The Next Exposure: The Trigger
When the person comes into contact with that allergen again, those IgE antibodies recognize it instantly. This sets off mast cells, which release histamine and other inflammatory chemicals into the bloodstream.
The Chain Reaction
Those chemicals cause:
Blood vessels to widen, which can drop blood pressure
Fluid to leak into surrounding tissues, causing swelling
Airways to tighten, making breathing difficult
Increased mucus production
In severe cases, strain on the heart
When breathing becomes compromised and blood pressure falls at the same time, the situation can turn critical very quickly.
Common Causes of Anaphylaxis
Anaphylaxis can be triggered by different allergens. The most common ones include:
Food Allergies
Peanuts
Tree nuts
Shellfish
Milk
Eggs
Soy
Wheat
Food-related anaphylaxis is especially common in children, though adults are also at risk.
Medications
Penicillin and other antibiotics
NSAIDs such as ibuprofen
Some chemotherapy drugs
Certain anesthesia medications
Insect Stings
Bees
Wasps
Hornets
Fire ants
Latex
Latex allergies are more common in healthcare workers or individuals who have had multiple surgeries.
Exercise-Induced Anaphylaxis
In rare cases, intense physical activity can trigger anaphylaxis—sometimes only if a specific food was eaten beforehand.
Idiopathic Anaphylaxis
Occasionally, no clear trigger can be identified, even after thorough evaluation.
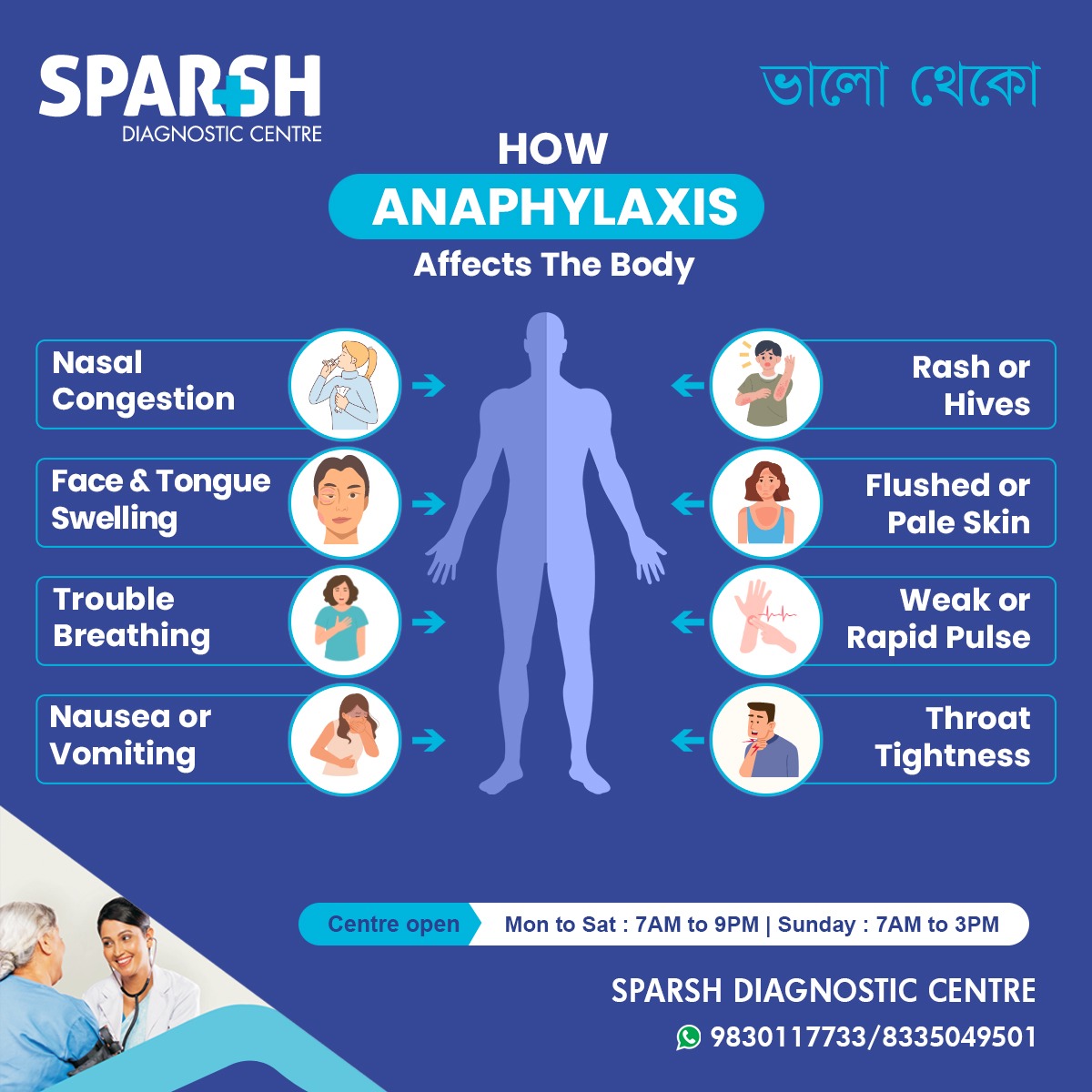
Signs and Symptoms of Anaphylaxis
Symptoms usually appear within minutes of exposure, though in some cases they may take longer.
Skin Symptoms (Most Common)
Hives
Itching
Flushed skin
Swelling of the lips, tongue, or throat
Breathing Problems
Chest tightness
Hoarse voice
Noisy breathing (stridor)
Heart and Circulation Changes
Digestive Symptoms
Neurological Symptoms
Confusion
A sudden sense that something is seriously wrong
One important clue doctors look for is involvement of more than one body system—for example, hives plus breathing difficulty—after exposure to a likely allergen.
When Does Anaphylaxis Become Life-Threatening?
Anaphylaxis becomes life-threatening when:
Swelling blocks the airway
Severe bronchospasm prevents oxygen from reaching the lungs
Blood pressure drops dangerously low (anaphylactic shock)
Serious heart rhythm disturbances develop
Anaphylactic shock is a type of distributive shock, meaning the blood vessels widen dramatically and fluid leaks out, leading to a collapse in circulation.
Emergency Treatment of Anaphylaxis
When it comes to anaphylaxis, speed matters.
1. Epinephrine Is the First and Most Important Step
Epinephrine (also called adrenaline) is the only medication that can quickly reverse the dangerous effects of anaphylaxis. It:
Tightens blood vessels to raise blood pressure
Relaxes airway muscles to improve breathing
Reduces swelling
Supports heart function
It should be injected into the outer thigh muscle as soon as anaphylaxis is suspected. Waiting too long to give epinephrine is one of the biggest risk factors for fatal outcomes.
2. Call Emergency Services Immediately
Even if symptoms improve after epinephrine, medical evaluation is still necessary. Reactions can return hours later.
3. Position the Person Properly
Lay them flat if possible
Elevate the legs if blood pressure is low
Avoid sudden standing
4. Hospital Treatment
In a medical setting, additional treatments may include:
Oxygen
IV fluids
Antihistamines
Inhaled medications for wheezing
These treatments can help, but they do not replace epinephrine.
What Is a Biphasic Reaction?
Sometimes, symptoms return after the initial reaction seems to have resolved. This is called a biphasic reaction.
It can occur within 1 to 72 hours, though most happen within the first 8–10 hours. That’s why observation in a hospital is often recommended after a serious episode.
Who Is at Higher Risk for Severe Anaphylaxis?
Certain factors increase the risk of a severe reaction:
A previous episode of anaphylaxis
Asthma, especially if poorly controlled
Use of beta-blocker medications
Delayed use of epinephrine
Children and young adults are particularly at risk for fatal reactions related to food allergies.
How Is Anaphylaxis Diagnosed?
Anaphylaxis is diagnosed based on symptoms and timing—there is no time to wait for lab tests in an emergency.
Blood tests, such as serum tryptase levels, may be checked later to confirm mast cell activation. Allergy testing is usually done afterward to identify the exact trigger.
Preventing Future Reactions
Once someone has experienced anaphylaxis, prevention becomes a top priority.
Avoid Known Triggers
Read food labels carefully
Inform restaurants about allergies
Be cautious in unfamiliar settings
Always Carry Epinephrine
Anyone diagnosed with anaphylaxis should carry an epinephrine auto-injector at all times. Ideally, they should:
Carry two doses
Check expiration dates regularly
Know exactly how to use it
Wear Medical Identification
A medical alert bracelet can provide critical information in an emergency.
Have a Written Action Plan
An allergy action plan should clearly outline:
Early warning signs
When to use epinephrine
Emergency contact steps
Consider Immunotherapy
For insect sting allergies, venom immunotherapy can significantly lower the risk of future severe reactions.
Anaphylaxis in Children
Children most commonly experience food-triggered anaphylaxis.
Schools play a key role in safety. Staff should be trained to recognize symptoms, and epinephrine should be easily accessible.
In infants, symptoms can be subtle. Watch for:
Unusual or persistent crying
Lethargy
Sudden vomiting
Limpness
Anaphylaxis vs. a Mild Allergic Reaction
Not every allergic reaction is anaphylaxis.
A mild reaction might involve a localized rash or mild itching with stable breathing and blood pressure. Anaphylaxis, on the other hand, typically includes breathing difficulty, widespread hives, low blood pressure, or multiple body systems being affected.
If there’s any doubt, it’s safer to treat it as anaphylaxis and use epinephrine.
Can Anaphylaxis Be Fatal?
Yes, it can.
Fatal cases often involve food allergies—especially peanuts and tree nuts—delayed epinephrine use, underlying asthma, or failure to recognize early warning signs.
The good news is that rapid treatment dramatically improves survival rates.
Living With the Risk of Anaphylaxis
Being diagnosed with anaphylaxis can be emotionally overwhelming. Many people worry about eating out, social gatherings, or accidental exposure.
But knowledge and preparation make a powerful difference. Understanding triggers, carrying epinephrine, and having a clear action plan can restore confidence and reduce anxiety.
Frequently Asked Questions
How quickly does anaphylaxis start?
Most reactions begin within minutes, though they can occasionally take up to an hour. Faster onset often means a more severe reaction.
Can antihistamines treat anaphylaxis?
No. They may ease itching or hives, but they do not treat airway swelling or shock. Epinephrine is essential.
Can a second dose of epinephrine be given?
Yes. If symptoms persist after 5–15 minutes, a second dose may be needed. Emergency care is still required.
Can anaphylaxis occur without hives?
Yes. Some people experience severe breathing or heart symptoms without any skin changes.
Is anaphylaxis inherited?
Allergies can run in families, but anaphylaxis itself is not directly inherited.
Can children outgrow food allergies?
Some children outgrow milk or egg allergies. Peanut and tree nut allergies are less likely to resolve but sometimes improve over time.
Should someone go to the hospital after using epinephrine?
Absolutely. Symptoms can return, and medical monitoring is important.
Can exercise cause anaphylaxis?
Yes. In rare cases, exercise—sometimes combined with certain foods—can trigger a reaction.
How should schools prepare?
By keeping emergency epinephrine available, training staff, creating clear action plans, and educating students about allergy safety.
Anaphylaxis is frightening—but it is manageable with the right knowledge and preparation. Recognizing symptoms early and using epinephrine without delay can save a life.
If you or someone close to you has experienced anaphylaxis, work with an allergy specialist to create a clear prevention and emergency plan.
Act quickly. Use epinephrine. Seek emergency care.
Those steps can make all the difference.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

Sparsh Diagnostic Centre Doctor List
![]()





