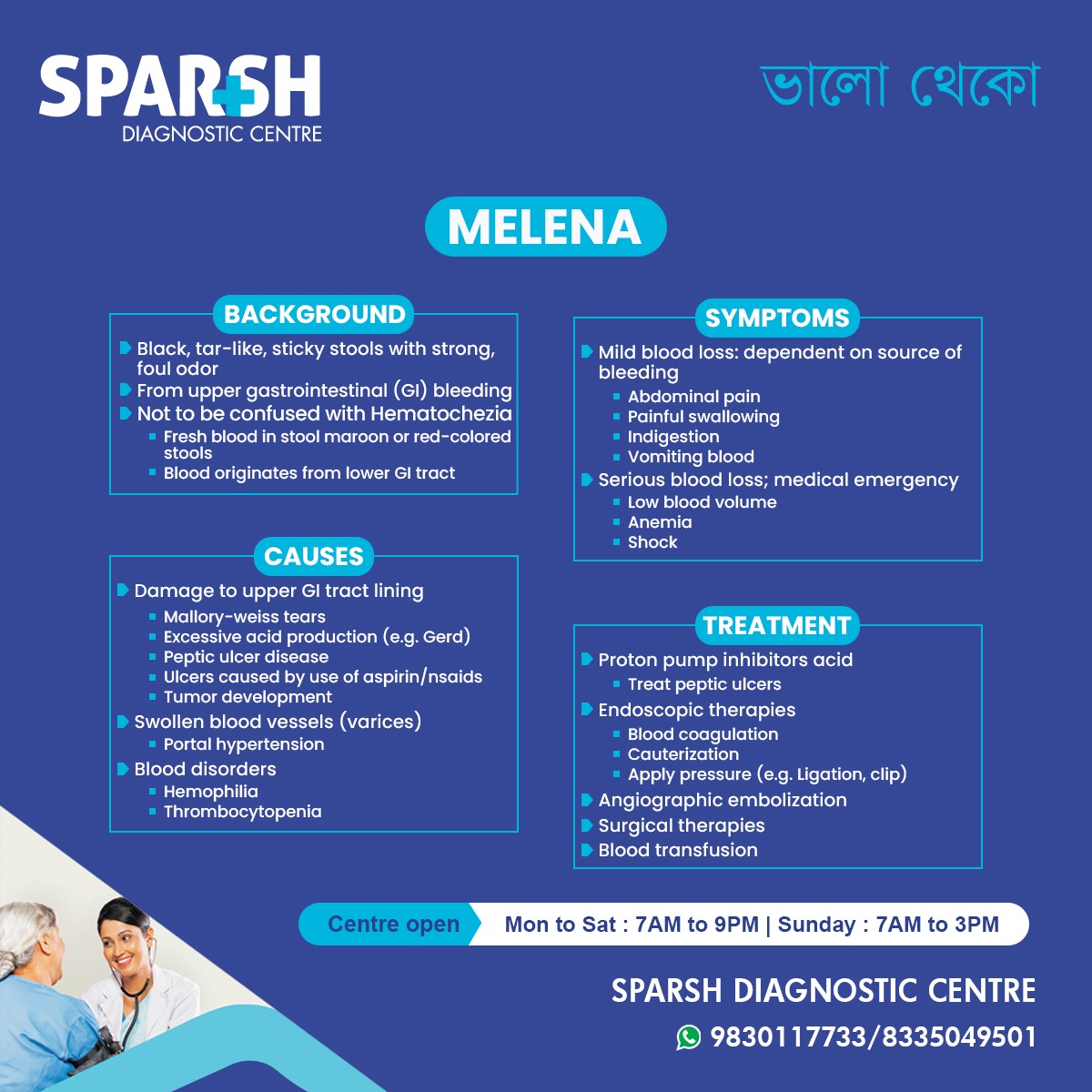
Melena is a clinical term used to describe black, tarry, sticky stools that carry a strong, foul odor. This condition typically indicates upper gastrointestinal (GI) bleeding, making it an important warning sign that should never be ignored. While many people confuse melena with hematochezia (fresh red blood in stool), both point to different types of bleeding and require different approaches to treatment. Understanding melena—its causes, symptoms, diagnostic methods, and treatment options—helps individuals seek timely care and prevent serious complications.
What is Melena?
Melena refers to dark, tar-like stools caused by the presence of digested blood. When bleeding occurs in the upper GI tract—such as the esophagus, stomach, or duodenum—the blood undergoes chemical changes as it travels through the digestive system. Enzymes and stomach acids break it down, turning it black and giving it a characteristic sticky consistency and pungent smell.
Because melena usually signals internal bleeding, it is considered a potentially serious condition.
Melena vs Hematochezia: Why the Difference Matters
Many people mistake melena for hematochezia, but understanding their distinction is crucial:
Melena
Black, tarry stools
Indicates upper GI bleeding
Blood is digested
Hematochezia
Bright red or maroon-colored blood in stool
Indicates lower GI bleeding (colon, rectum, anus)
Blood is fresh
Correct identification helps healthcare providers pinpoint the source of bleeding and initiate the right treatment strategy.
Common Causes of Melena
Several conditions can lead to bleeding in the upper GI tract. The most common include:
1. Peptic Ulcer Disease
Peptic ulcers are sores in the stomach or duodenal lining caused by:
Excess acid production
When these ulcers erode deeply, they can damage blood vessels and cause bleeding that leads to melena.
2. Gastritis
Inflammation of the stomach lining due to alcohol consumption, smoking, infections, or medications can result in bleeding.
3. Mallory-Weiss Tears
Repeated vomiting or severe coughing can cause tears in the esophagus–stomach junction, leading to bleeding.
4. Esophageal Varices
Swollen veins in the esophagus, often caused by liver diseases such as cirrhosis, may rupture and result in severe bleeding.
5. Tumors
Benign or malignant tumors in the stomach or upper small intestine can damage blood vessels and cause bleeding.
6. Use of Aspirin and NSAIDs
Regular use of painkillers like aspirin, ibuprofen, diclofenac, etc., increases the risk of GI mucosal injury and bleeding.
7. Coagulation Disorders
Conditions such as hemophilia, thrombocytopenia, or liver dysfunction impair blood clotting and increase the risk of bleeding.
Symptoms of Melena
Aside from black, tarry stools, melena often presents with symptoms related to blood loss.
Mild Bleeding Symptoms
Indigestion or bloating
Painful swallowing (depending on the source of bleeding)
Moderate to Severe Blood Loss Symptoms
When bleeding is significant, it becomes a medical emergency.
Symptoms include:
Low blood volume
Dizziness or fainting
Anyone experiencing these symptoms should seek urgent medical attention.
How Melena is Diagnosed
Doctors use several methods to confirm melena and determine its source.
1. Physical Examination
A detailed history and abdominal examination help identify possible causes and risk factors.
2. Stool Examination
A stool occult blood test (FOBT) can detect hidden blood.
3. Blood Tests
These help evaluate:
Hemoglobin levels
Blood clotting status
4. Endoscopy
Upper GI endoscopy is the gold standard for diagnosing and treating melena. It allows doctors to visualize the source of bleeding and perform immediate interventions.
5. Imaging Studies
In severe or unclear cases:
Capsule endoscopy
Radionuclide scans
These help locate bleeding sources that are difficult to detect with standard endoscopy.
Treatment Options for Melena
Treatment depends on the severity of bleeding and its underlying cause.
1. Medication Therapy
The goal is to reduce stomach acid, allow ulcers to heal, and stop bleeding.
Common medicines include:
Proton Pump Inhibitors (PPIs) like omeprazole or pantoprazole
H2 blockers
Antibiotics for H. pylori infections
Antacids for symptomatic relief
2. Endoscopic Treatment
Performed during an upper GI endoscopy. Options include:
Coagulation: Using heat or electricity to seal bleeding vessels
Cauterization
Hemostatic clipping: Applying metal clips to close bleeding vessels
Injection therapy: Epinephrine injections to constrict blood vessels
These treatments often stop bleeding immediately.
3. Angiographic Embolization
A radiologist identifies the bleeding vessel and blocks it using embolic materials. This is useful when endoscopy fails.
4. Surgical Intervention
Reserved for severe cases where:
Endoscopic therapy is ineffective
Tumors or large ulcers are involved
Surgeons may remove part of the stomach or repair damaged blood vessels.
5. Blood Transfusion
Patients with severe anemia or active bleeding may require transfusions to restore blood volume.
Risk Factors for Developing Melena
Certain lifestyle choices and medical conditions increase the risk of upper GI bleeding:
Chronic alcohol consumption
Long-term NSAID use
Smoking
Stress-related mucosal disease
Liver disease
Blood clotting disorders
Understanding these risk factors helps individuals take preventive steps.
Complications of Melena
If untreated, melena can lead to serious complications such as:
Severe anemia
Hypovolemic shock
Recurrent bleeding
Death (in extreme cases)
Timely diagnosis and treatment significantly reduce the chances of complications.
Preventive Measures
Although not all causes can be prevented, certain lifestyle modifications reduce the risk of upper GI bleeding.
1. Limit NSAID Use
Take painkillers only when prescribed and in recommended doses.
2. Avoid Alcohol and Smoking
Both irritate and damage the stomach lining.
3. Treat Acid Reflux Early
Uncontrolled GERD increases the risk of ulcers.
4. Manage Stress
Chronic stress is linked to stomach acid imbalance.
5. Maintain a Balanced Diet
Avoid spicy, fried, or acidic foods that irritate the stomach.
6. Follow Up Regularly
Patients with ulcers, liver disease, or bleeding disorders should undergo periodic check-ups.
When to See a Doctor
Seek medical help immediately if you experience:
Black, tarry stools
Blood in vomit
Persistent stomach pain
Dizziness, fainting, or rapid heartbeat
Unexplained fatigue
Known liver disease with new symptoms
Prompt treatment can save lives.
FAQ Section
1. Is melena always serious?
Yes. Melena indicates internal bleeding and should always be evaluated by a healthcare professional.
2. Can certain foods cause black stools?
Yes, foods like black licorice, blueberries, and iron supplements can darken stool, but they do not produce the tarry consistency and smell of melena.
3. Can melena go away on its own?
Not usually. The underlying cause of bleeding must be addressed to stop melena.
4. How is melena treated in emergencies?
Emergency treatment may involve IV fluids, blood transfusions, and endoscopic procedures to stop bleeding.
5. Can stress cause melena?
Stress alone doesn’t cause melena, but it can worsen conditions like gastritis or ulcers, increasing bleeding risk.
6. How long does melena last?
Once bleeding stops, it may take a few days for stools to return to normal color.
7. Can I prevent melena?
Yes. Lifestyle changes, avoiding NSAIDs, treating acid reflux, and regular check-ups can significantly reduce the risk.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()





[…] Dark, Tarry Stools: If gastritis leads to bleeding in the stomach, it can result in dark, tarry stools, a condition known as melena. This is a sign of more severe gastritis and requires immediate medical attention. […]
[…] Blood in the stool (melena) […]
[…] Dark or black stools (melena) suggest bleeding from the upper GI tract, such as the stomach or duodenum. […]