Hypovolemia is a serious medical condition characterized by a low extracellular fluid volume, often involving a significant loss of sodium and water. When the body loses more fluid than it takes in, blood volume drops, reducing the amount of blood circulating in the body. This can lead to reduced oxygen delivery to organs, life-threatening shock, and organ failure if not treated promptly.
Understanding hypovolemia is crucial because early recognition and timely medical care can prevent severe complications. This comprehensive guide explains everything you need to know—from causes and symptoms to diagnosis, treatment, and prevention.
What Is Hypovolemia?
Hypovolemia is a state of decreased blood volume, specifically the volume of blood plasma. Plasma is the liquid portion of blood that carries nutrients, hormones, and essential electrolytes like sodium and chloride.
When plasma volume drops, the body is unable to maintain adequate blood pressure, leading to decreased perfusion of vital organs such as the brain, kidneys, and heart. If left untreated, hypovolemia can progress to hypovolemic shock, a medical emergency.
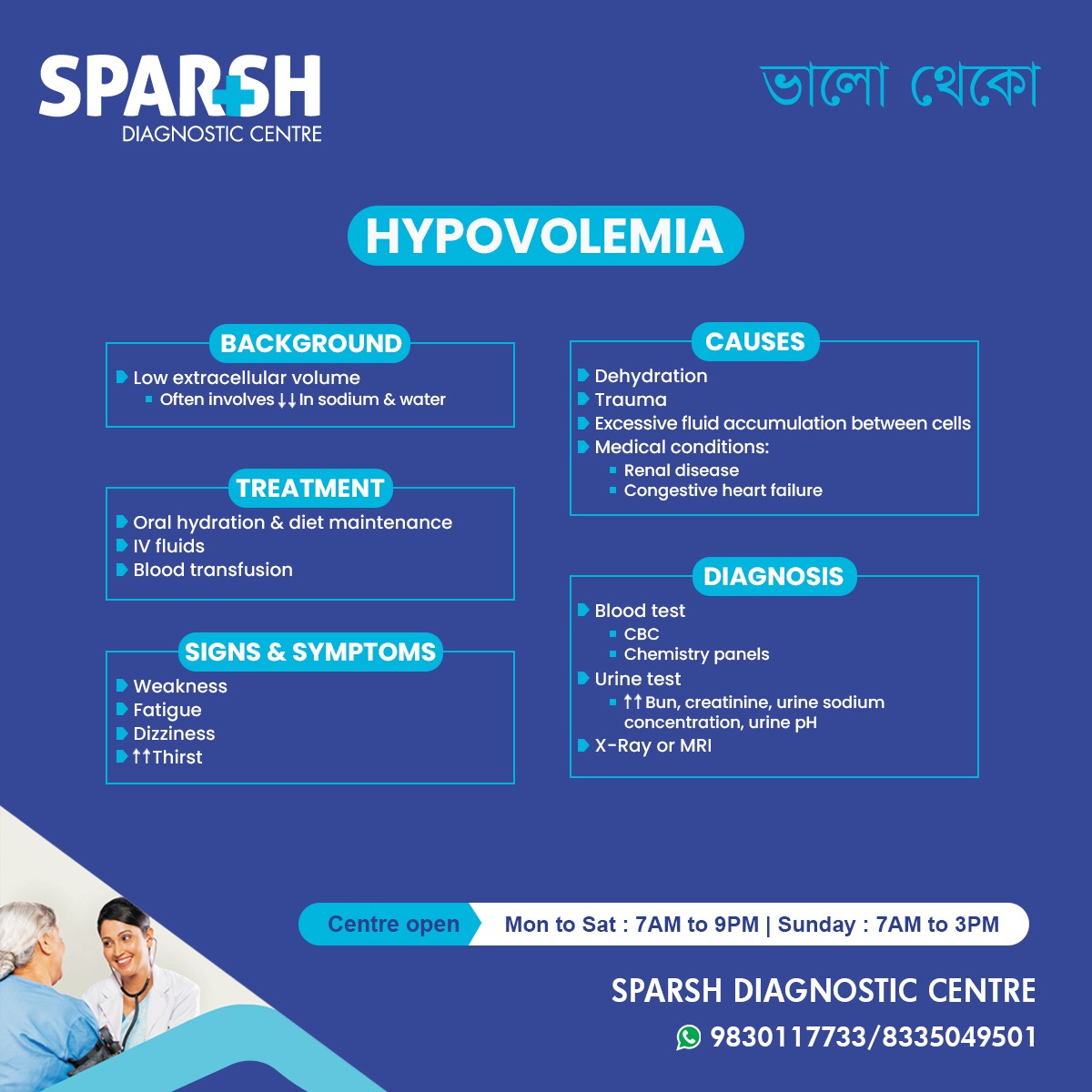
Background: Understanding Fluid Loss in Hypovolemia
The human body maintains a delicate fluid balance. Hypovolemia occurs when there is:
Low extracellular fluid volume
Often associated with ↓ sodium and ↓ water levels
This imbalance affects the body’s ability to maintain stable blood pressure and normal cellular function.
Extracellular fluid loss can result from:
Reduced water intake
Excessive water loss
Significant electrolyte imbalance
Internal or external bleeding
In severe cases, the body activates compensatory mechanisms—such as increased heart rate—to maintain circulation, but these mechanisms fail quickly if fluid loss continues.
Causes of Hypovolemia
Hypovolemia can develop from multiple underlying causes, which can generally be categorized into fluid loss, fluid redistribution, and medical conditions.
1. Dehydration
This is the most common cause. Dehydration can occur due to:
Dehydration leads to electrolyte loss along with water, worsening fluid imbalance.
2. Trauma
Traumatic injuries can cause:
External bleeding (e.g., cuts, accidents)
Internal bleeding (e.g., organ injury, ruptured blood vessels)
Both types lead to a rapid drop in circulatory volume.
3. Excessive Fluid Accumulation Between Cells
In some conditions, fluid leaks out of blood vessels into tissues, causing:
Reduced circulating blood volume
Although total body water remains the same, the effective circulating volume decreases.
4. Medical Conditions
Certain medical problems increase the risk of hypovolemia:
Renal disease
Kidneys fail to conserve fluids and electrolytes properly, causing excess loss through urine.
Congestive heart failure (CHF)
Though CHF often involves fluid overload, poor circulation may cause fluid to shift into tissues, reducing effective blood volume.
Signs and Symptoms of Hypovolemia
Hypovolemia symptoms vary depending on the severity of fluid loss. Early symptoms may be mild, but severe cases can rapidly become life-threatening.
Common Symptoms Include:
1. Weakness
Insufficient blood supply to muscles leads to fatigue and reduced energy levels.
2. Fatigue
Low blood volume affects oxygen delivery, making even simple activities exhausting.
3. Dizziness or Lightheadedness
This occurs due to low blood pressure and inadequate blood flow to the brain. It may worsen when standing—a condition known as orthostatic hypotension.
4. Increased Thirst
The body naturally triggers thirst to replenish lost fluids.
Additional Symptoms May Include:
Rapid, shallow breathing
Pale or cool skin
Reduced urine output
Confusion or irritability (especially in elderly patients)
Sunken eyes (in severe dehydration)
In advanced cases, hypovolemia can progress to shock, requiring immediate medical intervention.
Diagnosis of Hypovolemia
Proper diagnosis is essential to determine the extent of fluid loss and identify the underlying cause. Common diagnostic tests include:
1. Blood Tests
Blood tests help assess hydration status, electrolyte balance, and organ function.
CBC (Complete Blood Count)
Identifies anemia (from bleeding)
Helps detect infection or inflammation
Chemistry Panels
These measure key parameters such as:
Sodium
Potassium
Chloride
BUN and creatinine
Glucose levels
2. Urine Tests
Urine analysis provides insights into the kidneys’ response to dehydration.
Key indicators:
↑ BUN (Blood Urea Nitrogen)
↑ Creatinine
↑ Urine sodium concentration
Changes in urine pH
Dark yellow, concentrated urine often indicates dehydration.
3. Imaging (X-Ray or MRI)
These scans are used when internal bleeding or organ dysfunction is suspected.
X-rays help detect trauma or fractures
MRI provides detailed soft tissue imaging
Imaging is crucial when hypovolemia results from surgical complications, abdominal injuries, or organ bleeding.
Treatment of Hypovolemia
Treatment depends on the severity and cause of fluid loss. Early intervention dramatically improves outcomes.
1. Oral Hydration & Diet Maintenance
For mild hypovolemia, treatment includes:
Oral rehydration solutions (ORS)
Increased water intake
Electrolyte-rich fluids
Balanced diet
Avoiding caffeine and alcohol (they worsen dehydration)
ORS is particularly effective because it restores both fluids and electrolytes.
2. IV (Intravenous) Fluids
Moderate to severe hypovolemia requires IV fluids like:
Normal saline
Ringer’s lactate solution
These fluids quickly restore circulatory volume and correct electrolyte imbalance.
3. Blood Transfusion
In cases of traumatic injury or severe bleeding, blood transfusion is necessary to restore both blood cells and plasma volume.
Transfusions help:
Improve oxygen delivery
Stabilize blood pressure
Replace lost hemoglobin
4. Medications
Depending on the underlying cause:
Antibiotics for infections
Anti-diarrheal or antiemetic medications
Vasopressors to support blood pressure in severe cases
5. Treating the Underlying Cause
Long-term management involves addressing:
Kidney disorders
Trauma or bleeding sources
Complications of Untreated Hypovolemia
If left unaddressed, hypovolemia can lead to serious health consequences, including:
Because of these risks, prompt diagnosis and treatment are essential.
Preventing Hypovolemia
While some causes are unavoidable, many cases can be prevented with simple measures:
Hydration
Drink adequate water daily
Increase fluid intake during hot weather or exercise
Monitor Fluid Loss
Address vomiting or diarrhea immediately
Avoid overuse of diuretics
Manage Chronic Conditions
Regular check-ups help detect early complications of kidney disease or heart failure.
Healthy Diet
Maintain electrolyte balance
Include fruits, vegetables, soups, and fluids
First Aid Awareness
Respond quickly to bleeding injuries by applying pressure and seeking medical care.
Hypovolemia in High-Risk Groups
Certain populations are more vulnerable to fluid loss:
1. Children and Infants
They dehydrate faster than adults due to higher metabolic rates.
2. Older Adults
They may have reduced thirst sensation and underlying chronic conditions.
3. Athletes
Intense physical activity leads to excessive sweating.
4. People with Chronic Illnesses
Renal disease, diabetes, and heart failure increase the risk of fluid imbalance.
When to See a Doctor
Seek immediate medical attention if you notice:
Persistent dizziness
Severe fatigue
Very low urine output
Rapid heartbeat
Confusion
Any signs of bleeding
Hypovolemia can escalate quickly, especially in children and elderly individuals.
FAQ Section
1. What is the main cause of hypovolemia?
Dehydration is the most common cause, often triggered by vomiting, diarrhea, sweating, or inadequate fluid intake. Trauma and bleeding are also major contributors.
2. How can you tell if someone is hypovolemic?
Symptoms such as dizziness, weakness, low urine output, rapid heart rate, and increased thirst are common signs. Severe cases may show confusion and low blood pressure.
3. Can hypovolemia be treated at home?
Mild hypovolemia can be managed with oral rehydration and rest. However, moderate to severe cases require medical attention and IV fluids.
4. What is the difference between hypovolemia and dehydration?
Dehydration refers specifically to loss of water, while hypovolemia refers to loss of blood volume, which includes both water and electrolytes—and sometimes blood cells.
5. How quickly can hypovolemia become serious?
It can become dangerous within minutes in cases of trauma or bleeding. In dehydration-related hypovolemia, progression may occur over hours or days.
6. What tests confirm hypovolemia?
Doctors may perform blood tests, urine tests, and imaging studies (X-ray or MRI) to determine fluid loss and assess organ function.
7. Is hypovolemia life-threatening?
Yes. Severe hypovolemia can lead to hypovolemic shock, organ failure, and death if not treated promptly.
Hypovolemia is a major medical concern that requires timely diagnosis and intervention. Whether caused by dehydration, bleeding, trauma, or chronic illness, early recognition of symptoms can prevent severe complications.
Sparsh Diagnostic Centre offers comprehensive diagnostic services such as CBC, chemistry panels, urine tests, advanced imaging modalities to accurately diagnose and manage hypovolemia. If you notice any early signs, do not delay seeking medical help—your health and safety depend on timely action.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()





