Wolff–Parkinson–White (WPW) Syndrome is a congenital cardiac conduction disorder that can lead to episodes of rapid heart rhythm (tachyarrhythmia). Although many individuals with WPW syndrome may remain asymptomatic throughout life, others can experience palpitations, dizziness, chest discomfort, or even life-threatening arrhythmias.
Early detection through electrocardiography (ECG) and appropriate evaluation plays a critical role in preventing complications. This article provides an in-depth overview of WPW syndrome, including its causes, symptoms, ECG features, diagnostic tests, treatment options, and long-term outlook.
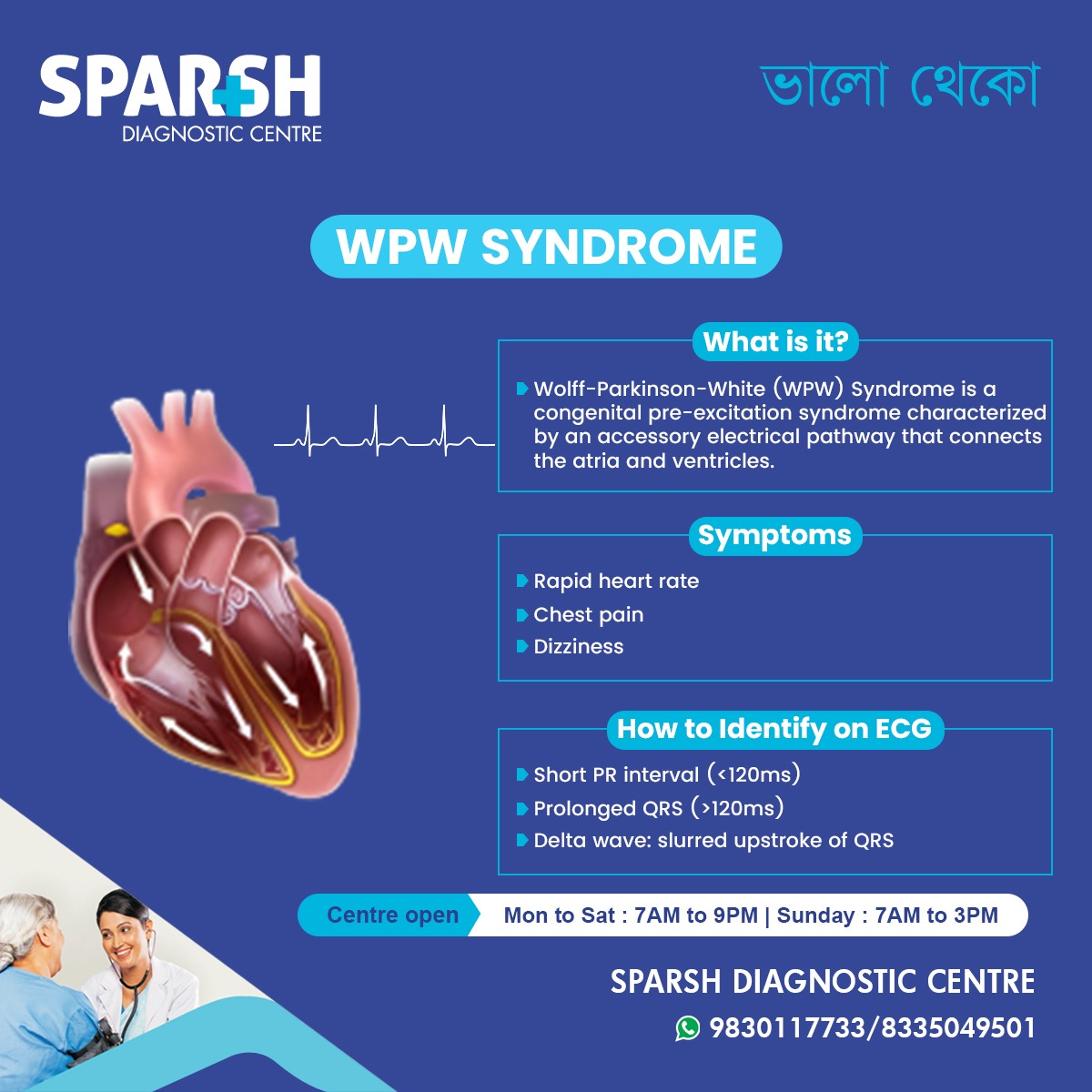
What is Wolff–Parkinson–White (WPW) Syndrome?
Wolff–Parkinson–White syndrome is a pre-excitation syndrome of the heart. It occurs due to the presence of an extra electrical pathway, known as an accessory pathway, between the atria and ventricles.
Under normal conditions, electrical impulses travel from the atria to the ventricles through the atrioventricular (AV) node. In WPW syndrome, the accessory pathway allows electrical signals to bypass the AV node, causing early activation (pre-excitation) of the ventricles.
This abnormal conduction can result in rapid heart rhythms, particularly supraventricular tachycardia (SVT).
WPW Syndrome vs WPW Pattern
It is important to distinguish between:
WPW Pattern: Characteristic ECG findings without symptoms
WPW Syndrome: ECG findings plus symptoms related to tachyarrhythmias
Many individuals have a WPW pattern incidentally detected on ECG but never develop clinical symptoms.
Causes of WPW Syndrome
WPW syndrome is a congenital condition, meaning it is present at birth.
Key Causes and Associations
Abnormal development of cardiac conduction tissue during fetal life
Presence of one or more accessory pathways (Bundle of Kent)
Rare genetic associations (familial WPW syndrome)
Association with congenital heart disease such as:
Ebstein’s anomaly
Hypertrophic cardiomyopathy (rare)
In most cases, WPW syndrome occurs sporadically without a clear family history.
Pathophysiology: How does WPW Syndrome affect the Heart
The accessory pathway allows electrical impulses to travel:
From atria to ventricles faster than normal
In both directions (anterograde or retrograde)
This sets up a re-entry circuit, leading to episodes of rapid heart rate. The most common arrhythmias associated with WPW syndrome include:
Atrioventricular re-entrant tachycardia (AVRT)
Atrial fibrillation with rapid ventricular response (dangerous in WPW)
Symptoms of WPW Syndrome
Symptoms can vary widely, from mild palpitations to severe cardiovascular events.
Common Symptoms
Severe or Emergency Symptoms
Symptoms may occur at rest or be triggered by exercise, stress, caffeine, or alcohol.
WPW Syndrome in Children and Infants
WPW syndrome can present at any age, including infancy.
Pediatric Symptoms
Poor feeding
Irritability
Pallor
Failure to thrive
Early diagnosis in children is important to prevent complications and guide long-term management.
How Is WPW Syndrome diagnosed?
1. Electrocardiogram (ECG)
ECG is the cornerstone of diagnosis.
Classic ECG Features of WPW Syndrome
Short PR interval (<120 ms)
Delta wave (slurred upstroke of the QRS complex)
Wide QRS complex (>120 ms)
Secondary ST-T wave changes
These findings reflect early ventricular activation through the accessory pathway.
2. Holter Monitoring
A 24-hour or longer Holter monitor may be used to:
Detect intermittent pre-excitation
Identify arrhythmia episodes
Correlate symptoms with heart rhythm
3. Event Recorder or Loop Recorder
Used when symptoms are infrequent but concerning.
4. Echocardiography
Helps evaluate:
Structural heart disease
Cardiac function
Associated congenital abnormalities
5. Electrophysiology (EP) Study
An invasive but definitive test that:
Identifies location of accessory pathway
Assesses arrhythmia risk
Guides catheter ablation therapy
Risk Stratification in WPW Syndrome
Not all patients with WPW syndrome have the same risk.
High-Risk Features
History of syncope
Documented atrial fibrillation
Very rapid ventricular rates
Multiple accessory pathways
Short refractory period of the pathway
Risk assessment is especially important in young individuals and athletes.
Treatment Options for WPW Syndrome
Treatment depends on symptom severity, arrhythmia risk, and patient age.
1. Observation and Monitoring
For asymptomatic individuals:
Regular follow-up
Patient education on warning signs
2. Medications
Antiarrhythmic drugs may be used to control heart rhythm.
Commonly Used Medications
Beta-blockers
Calcium channel blockers (with caution)
Antiarrhythmic agents such as flecainide or propafenone
⚠️ Certain drugs are contraindicated in WPW with atrial fibrillation, as they may worsen ventricular response.
3. Catheter Ablation (Definitive Treatment)
Radiofrequency catheter ablation is the treatment of choice for symptomatic WPW syndrome.
Advantages
High success rate (>95%)
Minimally invasive
Low complication rate
Potentially curative
During the procedure, the accessory pathway is precisely located and destroyed using radiofrequency energy or cryoablation.
WPW Syndrome and Emergency Management
Acute Tachycardia Management
Vagal maneuvers (Valsalva, carotid massage – under supervision)
Intravenous antiarrhythmic drugs
Electrical cardioversion if unstable
⚠️ AV nodal blocking agents (e.g., digoxin, verapamil) should be avoided in WPW with atrial fibrillation.
Lifestyle Considerations for Patients with WPW Syndrome
Avoid excessive caffeine and stimulants
Limit alcohol intake
Manage stress
Stay hydrated
Adhere to follow-up schedules
Athletes may require specialized evaluation before competitive sports participation.
Prognosis of WPW Syndrome
With early diagnosis and appropriate treatment:
Most individuals live normal, healthy lives
Catheter ablation offers excellent long-term outcomes
Risk of sudden cardiac death is low but not negligible without evaluation
Regular monitoring ensures optimal safety and quality of life.
When Should You See a Doctor?
Seek medical attention if you experience:
Recurrent palpitations
Fainting episodes
Chest pain
Rapid heartbeat at rest
Family history of sudden cardiac death
Early ECG screening can be lifesaving.
Role of Sparsh Diagnostic Centre in WPW Syndrome
Sparsh plays a key role by offering:
Holter and ambulatory monitoring
Echocardiography
Timely referrals for electrophysiology evaluation
Accurate diagnosis is the first step toward effective treatment.
Frequently Asked Questions (FAQ)
1. Is it dangerous?
WPW syndrome can be serious if left undiagnosed, especially in symptomatic patients. However, with proper evaluation and treatment, the prognosis is excellent.
2. Can it go away on its own?
The accessory pathway does not disappear spontaneously. Symptoms may fluctuate, but the condition persists unless treated with catheter ablation.
3. Is it hereditary?
Most cases are sporadic, but rare familial forms exist. Genetic testing is not routinely required.
4. Can it cause sudden cardiac death?
The risk is low but present, particularly in individuals with atrial fibrillation and rapid ventricular response. Risk stratification is essential.
5. Can people with WPW syndrome exercise?
Many individuals can exercise safely after proper evaluation. Competitive athletes may need additional testing before clearance.
6. How is it detected?
WPW syndrome is primarily diagnosed through an ECG showing short PR interval, delta wave, and wide QRS complex.
7. Is catheter ablation safe?
Yes. It is a well-established procedure with high success and low complication rates when performed by experienced specialists.
8. Can it affect children?
Yes. WPW can occur in infants and children and may present with feeding difficulty or rapid heart rate.
9. Do all patients need treatment?
No. Asymptomatic patients may only require observation, while symptomatic or high-risk patients benefit from ablation.
10. Can it be cured?
Catheter ablation can permanently eliminate the accessory pathway, effectively curing the condition.
To consult a Cardiologist at Sparsh Diagnostic Centre for treatment of Wolff–Parkinson–White Syndrome, call our helpline number 9830117733.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

Sparsh Doctor List
![]()