Proximal neuropathy is a rare but serious type of nerve disorder that primarily affects the nerves in the hips, thighs, buttocks, and sometimes the shoulders and upper arms. Unlike more common peripheral neuropathies that start in the hands or feet, proximal neuropathy involves nerves closer to the center of the body, often causing severe pain, muscle weakness, and difficulty with everyday movements such as standing, walking, or climbing stairs.
This condition is most frequently associated with diabetes but can also occur due to autoimmune diseases, infections, inflammatory conditions, or nerve ischemia. Early diagnosis and appropriate treatment play a crucial role in improving outcomes and reducing long-term disability.
This comprehensive guide explains proximal neuropathy in detail, including its causes, symptoms, diagnostic approach, treatment options, recovery expectations, and frequently asked questions.
What Is Proximal Neuropathy?
Proximal neuropathy, also known as diabetic amyotrophy or lumbosacral radiculoplexus neuropathy, is a form of nerve damage that affects the proximal (near-center) muscles of the body. It most commonly involves:
Hips
Thighs
Buttocks
Lower back
Occasionally shoulders and upper arms
The condition typically begins suddenly with intense pain on one side of the body, followed by progressive muscle weakness and muscle wasting.
Types of Proximal Neuropathy
1. Diabetic Proximal Neuropathy
This is the most common form and occurs in people with type 2 diabetes, though it can also affect those with type 1 diabetes. Interestingly, it may develop even in individuals with relatively well-controlled blood sugar levels.
2. Non-Diabetic Proximal Neuropathy
This form may be caused by:
Infections
Idiopathic (unknown causes)
Causes of Proximal Neuropathy
The exact mechanism of proximal neuropathy is not always fully understood, but several contributing factors have been identified.
Common Causes Include:
Diabetes mellitus – most frequent cause
Reduced blood supply (ischemia) to nerves
Infections affecting nerve roots or plexus
Post-viral immune reactions
Paraneoplastic syndromes (associated with cancer)
In diabetic cases, the condition is believed to be caused more by immune-mediated inflammation and microvascular damage rather than direct effects of high blood sugar alone.
Symptoms of Proximal Neuropathy
Symptoms often develop rapidly and may progress over weeks or months. They are usually more severe than those seen in distal neuropathies.
Common Symptoms Include:
Severe pain in the buttock, hip, or thigh
Sudden onset of one-sided pain, later becoming bilateral in some cases
Weakness in thigh and hip muscles
Difficulty standing up from a seated position
Trouble climbing stairs
Muscle wasting or shrinking (atrophy)
Lower back pain
Reduced knee reflexes
Weight loss (commonly seen in diabetic amyotrophy)
Fatigue and reduced mobility

In advanced cases, patients may require walking aids or assistance with daily activities.
How Proximal Neuropathy Differs from Other Neuropathies
| Feature | Proximal Neuropathy | Peripheral Neuropathy |
|---|---|---|
| Affected area | Hips, thighs, buttocks | Feet, hands |
| Pain severity | Severe | Mild to moderate |
| Muscle weakness | Prominent | Less prominent |
| Onset | Sudden or subacute | Gradual |
| Common cause | Diabetes, inflammation | Diabetes, toxins |
Diagnosis of Proximal Neuropathy
Diagnosing proximal neuropathy requires a combination of clinical evaluation, laboratory testing, and imaging to rule out other neurological conditions.
Clinical Evaluation
A neurologist or physician will assess:
Pain pattern and progression
Muscle strength
Reflexes
Sensory changes
Gait and posture
Diagnostic Tests
1. Blood Tests
Blood glucose and HbA1c
Inflammatory markers
Vitamin deficiencies
Autoimmune markers
2. Nerve Conduction Studies (NCS)
Measures the speed and strength of electrical signals in nerves.
3. Electromyography (EMG)
Evaluates muscle activity and confirms nerve involvement.
4. MRI of Spine or Pelvis
Helps exclude:
Tumors
Structural compression
5. Cerebrospinal Fluid (CSF) Analysis
May show elevated protein levels in inflammatory cases.
Treatment of Proximal Neuropathy
Treatment focuses on relieving pain, managing the underlying cause, restoring strength, and preventing complications.
1. Pain Management
Neuropathic pain medications (gabapentin, pregabalin)
Tricyclic antidepressants
Short-term opioids (in severe cases, under supervision)
2. Blood Sugar Control (in Diabetic Patients)
Optimizing glucose levels
Regular monitoring
Medication adjustments
3. Immunotherapy (Selected Cases)
For inflammatory or autoimmune causes:
Intravenous immunoglobulin (IVIG)
Immunosuppressive medications
4. Physical Therapy
Strengthening exercises
Gait training
Balance improvement
Prevention of muscle wasting
5. Nutritional Support
Adequate protein intake
Correction of vitamin deficiencies
Weight stabilization
Recovery and Prognosis
The good news is that proximal neuropathy is often self-limiting, meaning symptoms gradually improve over time.
What to Expect:
Pain usually improves first
Muscle strength recovery may take months to years
Most patients show significant improvement within 6–18 months
Some residual weakness may persist
Early diagnosis and rehabilitation significantly improve long-term outcomes.
Complications of Untreated Proximal Neuropathy
If left untreated, proximal neuropathy may lead to:
Severe muscle wasting
Long-term disability
Increased fall risk
Dependence on walking aids
Reduced quality of life
Prevention Tips
While not all cases can be prevented, certain measures reduce risk:
Manage autoimmune conditions effectively
Maintain healthy body weight
Seek early medical attention for unexplained nerve pain
Follow up regularly with healthcare providers
When to See a Doctor
Seek medical evaluation if you experience:
Sudden severe hip or thigh pain
Progressive leg weakness
Difficulty walking or standing
Unexplained weight loss with nerve pain
Symptoms worsening over weeks
Early intervention can prevent complications and speed recovery.
Frequently Asked Questions (FAQ)
1. Is proximal neuropathy the same as sciatica?
No. Sciatica is caused by nerve root compression, while proximal neuropathy is typically due to nerve inflammation or ischemia.
2. Can proximal neuropathy occur without diabetes?
Yes. Although diabetes is the most common cause, it can also occur due to autoimmune, infectious, or idiopathic reasons.
3. Is proximal neuropathy reversible?
In many cases, yes. Most patients experience partial to significant recovery over time with appropriate treatment.
4. How long does recovery take?
Recovery may take several months to up to two years, depending on severity and underlying cause.
5. Is proximal neuropathy life-threatening?
No, but it can significantly affect mobility and quality of life if not treated.
6. Does proximal neuropathy affect both legs?
It often starts on one side but may eventually affect both sides.
7. What tests confirm proximal neuropathy?
EMG, nerve conduction studies, blood tests, and imaging studies are commonly used.
8. Can exercise help proximal neuropathy?
Yes. Supervised physical therapy helps restore strength and prevent muscle wasting.
9. Is surgery required for proximal neuropathy?
Surgery is rarely required unless another structural cause is identified.
10. Can proximal neuropathy recur?
Recurrence is uncommon but possible, especially if underlying conditions are not well controlled.
Proximal neuropathy is a painful and disabling nerve condition that primarily affects the hips and thighs, most often in individuals with diabetes. While symptoms can be severe, early diagnosis, appropriate treatment, and rehabilitation significantly improve outcomes. With proper care, most patients regain strength, mobility, and independence over time.
If you or a loved one experiences unexplained hip or thigh pain with weakness, prompt medical evaluation is essential for accurate diagnosis and timely management.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
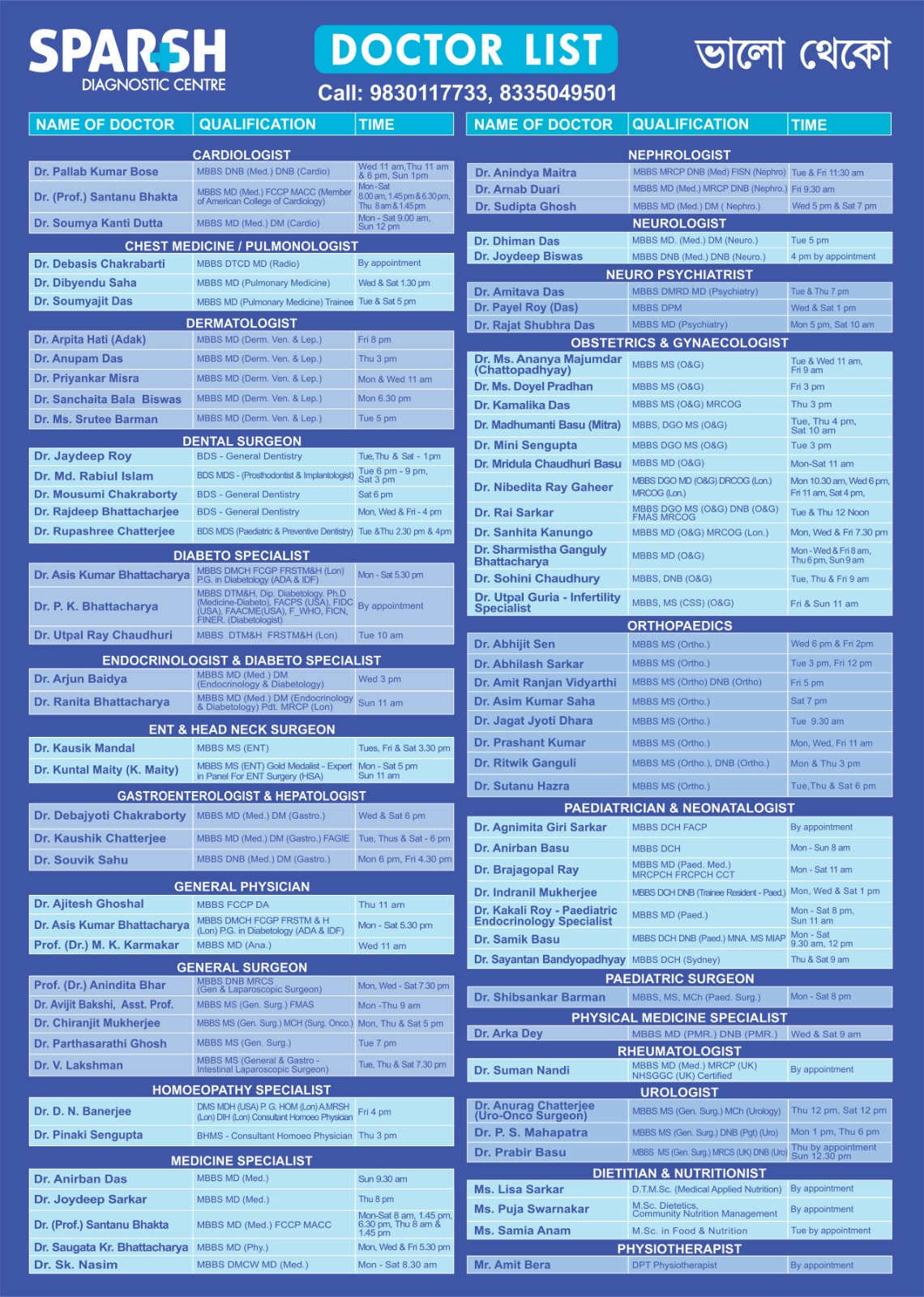
Sparsh Doctor List
![]()