Postural Orthostatic Tachycardia Syndrome (POTS) is a complex condition that affects blood circulation (autonomic nervous system), leading to a rapid increase in heart rate when standing up from a sitting or lying position. Although not life-threatening, POTS can severely impact quality of life, causing fatigue, dizziness, and even fainting. Understanding this condition is the first step toward effective management and recovery.
What Is Postural Orthostatic Tachycardia Syndrome (POTS)?
POTS is a type of dysautonomia, a disorder of the autonomic nervous system (ANS). The ANS regulates automatic body functions such as heart rate, blood pressure, and temperature control.
When someone with POTS stands up, blood pools in the lower body instead of circulating efficiently to the brain and heart.
To compensate, the heart beats faster—often by 30 beats per minute or more within 10 minutes of standing—but blood flow to the brain still drops, leading to light-headedness, palpitations, and fatigue.
POTS predominantly affects women aged 15–50 years, though it can occur in men and children as well.
Types of POTS
There are several subtypes of POTS, each with different underlying mechanisms:
Neuropathic POTS – Caused by nerve damage that prevents proper blood vessel constriction in the lower limbs.
Hyperadrenergic POTS – Associated with high levels of norepinephrine (a stress hormone), leading to excessive heart rate and anxiety-like symptoms.
Hypovolemic POTS – Characterized by low blood volume, leading to decreased blood flow to vital organs.
Secondary POTS – Develops due to another medical condition, such as diabetes, lupus, or after a viral infection.
Common Symptoms of POTS
Symptoms of POTS can vary in severity and may worsen upon standing or prolonged inactivity. Key symptoms include:
Shaking and sweating
Fainting or near-fainting episodes
Poor sleep or insomnia
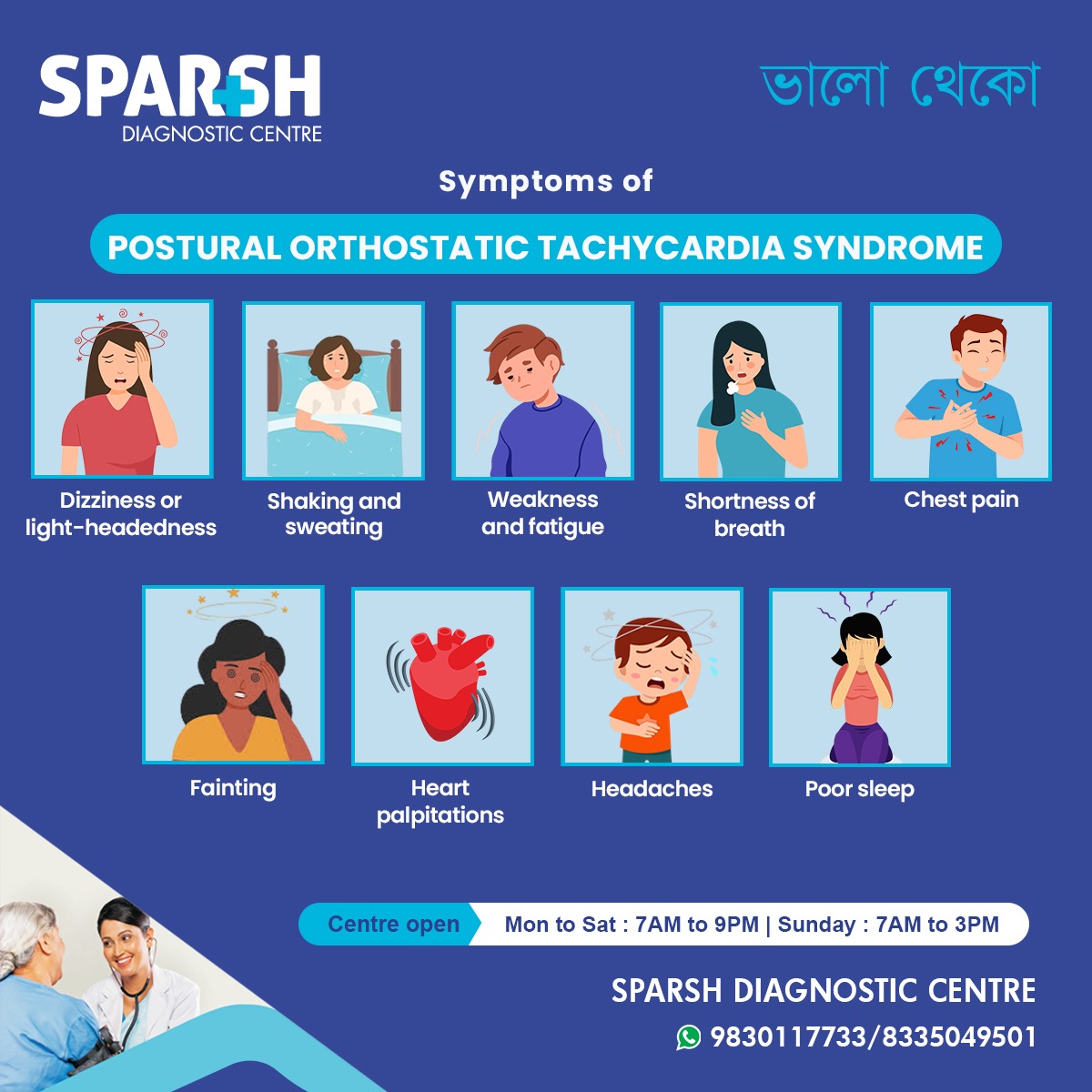
Other possible symptoms include blurred vision, nausea, brain fog, anxiety, temperature sensitivity, and difficulty concentrating.
Causes and Risk Factors
While the exact cause of POTS is not fully understood, several factors may contribute to its development:
Genetic predisposition – A family history of autonomic disorders or fainting spells increases risk.
Viral infections – Many patients develop POTS after a viral illness, such as mononucleosis, flu, or COVID-19.
Autoimmune conditions – Diseases like lupus, Sjögren’s syndrome, or Hashimoto’s thyroiditis can trigger POTS.
Physical deconditioning – Long periods of bed rest or inactivity may lead to POTS symptoms.
Hormonal changes – POTS is more common in women, suggesting a link with estrogen and hormonal fluctuations.
Low blood volume (hypovolemia) – Insufficient circulating blood volume can contribute to symptoms.
How does POTS affect the body
When standing, gravity pulls blood to the legs and abdomen. Normally, blood vessels constrict to push blood back to the heart and brain. In POTS, this mechanism fails — leading to reduced blood flow to the brain and increased heart rate as the body compensates.
This imbalance can cause symptoms that interfere with daily life, including extreme fatigue after minor exertion, brain fog, and difficulty standing for long periods.
Diagnosis of POTS
Diagnosis typically involves a thorough medical history, physical examination, and autonomic testing.
1. Tilt Table Test
This is the gold-standard diagnostic test. The patient lies on a table that tilts upright while heart rate and blood pressure are monitored. A heart rate increase of at least 30 beats per minute (or exceeding 120 bpm) within 10 minutes of standing indicates POTS.
2. Active Stand Test
Similar to the tilt table test but performed manually. Measurements are taken while lying down and after standing for several minutes.
3. Blood and Urine Tests
To rule out conditions like anemia, thyroid disease, or electrolyte imbalance.
4. Autonomic Function Tests
These assess how the autonomic nervous system responds to changes in posture, temperature, and breathing.
5. Echocardiogram and ECG
These help rule out structural heart disease or arrhythmias.
Treatment and Management of POTS
While there is no cure for POTS, treatment focuses on symptom control, improving blood flow, and enhancing quality of life. A combination of lifestyle changes, medications, and physical therapy is often most effective.
1. Lifestyle Modifications
Increase fluid intake: Aim for 2–3 litres of water daily.
Boost salt intake: Sodium helps retain fluid and raise blood pressure.
Compression garments: Wearing waist-high compression stockings prevents blood pooling in the legs.
Avoid prolonged standing: Take breaks or sit when possible.
Elevate head during sleep: Improves blood circulation and reduces morning dizziness.
2. Exercise and Physical Therapy
Graded exercise programs—starting with recumbent biking, rowing, or swimming—help rebuild muscle tone and improve circulation. Patients should increase activity levels slowly to avoid symptom flare-ups.
3. Medications
Depending on symptoms, doctors may prescribe:
Fludrocortisone – Helps the body retain sodium and water.
Midodrine – Constricts blood vessels to increase blood pressure.
Beta-blockers – Control heart rate and reduce palpitations.
Ivabradine – Lowers heart rate without lowering blood pressure.
SSRIs or SNRIs – For patients with coexisting anxiety or depression.
All medications should be used only under medical supervision.
4. Dietary Adjustments
Eat small, frequent meals to avoid post-meal dizziness.
Avoid caffeine and alcohol, which can worsen dehydration.
Increase potassium and magnesium intake through fruits and vegetables.
5. Psychological Support
POTS can lead to anxiety, frustration, and depression. Cognitive-behavioral therapy (CBT) and support groups can help patients cope with chronic symptoms.
Living with POTS
Although POTS can be challenging, many patients see improvement with time, especially with early diagnosis and consistent management. Adopting a balanced approach that includes hydration, salt intake, physical reconditioning, and emotional support can dramatically enhance daily functioning.
Patients should maintain regular follow-ups with their physician and monitor any symptom changes, particularly heart rate, fatigue levels, and dizziness.
Complications of POTS
Untreated or poorly managed POTS can lead to:
Frequent fainting and falls
Chronic fatigue and deconditioning
Difficulty working or attending school
Psychological distress (anxiety, depression)
However, POTS does not typically cause heart damage or shorten lifespan when properly managed.
Prevention Tips
While POTS itself may not always be preventable, certain strategies can help reduce flare-ups:
Stay hydrated throughout the day.
Include enough salt in your diet (as advised by your doctor).
Perform regular light exercises to maintain muscle strength.
Avoid sudden posture changes (e.g., getting up too quickly).
Manage stress effectively through meditation or yoga.
When to See a Doctor
Seek medical attention if you experience:
Persistent dizziness or fainting upon standing
Rapid heartbeat that doesn’t subside
Shortness of breath or chest discomfort
Extreme fatigue interfering with daily activities
Early diagnosis and care can help identify POTS accurately and start timely treatment.
FAQ on Postural Orthostatic Tachycardia Syndrome (POTS)
1. Is POTS a heart problem?
Not exactly. POTS primarily affects the autonomic nervous system, not the heart muscle itself. However, it causes changes in heart rate that mimic heart conditions.
2. Can POTS be cured?
There is currently no permanent cure, but most people experience significant improvement through lifestyle changes and treatment.
3. Is POTS related to anxiety?
While symptoms may resemble anxiety (like palpitations and sweating), POTS is a physiological condition, not a psychological one.
4. Can dehydration trigger POTS symptoms?
Yes. Dehydration reduces blood volume, worsening dizziness and rapid heart rate.
5. How long does it take to recover from POTS?
Recovery varies. Some improve within months, while others manage chronic symptoms over years with consistent care.
6. Can exercise help POTS patients?
Yes, graded exercise can improve circulation and muscle strength, reducing symptoms over time.
7. Is POTS linked to COVID-19?
Recent studies suggest that some long COVID patients develop POTS-like symptoms due to autonomic dysfunction after viral infection.
👉 For accurate diagnosis and expert guidance on POTS, visit Sparsh Diagnostic Centre
📞 Call 9830117733 / 8335049501 to book your appointment.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()





[…] 2. Postural Orthostatic Tachycardia Syndrome (POTS) […]
[…] Postural Orthostatic Tachycardia Syndrome (POTS): […]