Campylobacter infection, also known as campylobacteriosis, is one of the most common bacterial causes of foodborne illness worldwide. The infection is primarily caused by Campylobacter jejuni and Campylobacter coli, bacteria that infect the intestinal tract and lead to gastrointestinal distress.
Although most cases are mild and resolve within a week, severe infections can cause complications, especially in infants, the elderly, and people with weakened immune systems. Early diagnosis and proper hydration are key to recovery.
What Is Campylobacter Infection?
Campylobacter infection occurs when a person ingests food, water, or raw animal products contaminated with Campylobacter bacteria. It affects the gastrointestinal tract, leading to diarrhea, fever, abdominal cramps, and other systemic symptoms.
How Does Campylobacter Spread?
The infection is usually transmitted through the fecal-oral route. This means that bacteria from animal or human feces contaminate food or water, which, when consumed, infect the digestive tract.
Common sources of infection include:
Undercooked poultry – especially chicken and turkey.
Unpasteurized milk or dairy products.
Contaminated drinking water.
Contact with infected animals (especially farm animals or pets).
Cross-contamination from raw meat during food preparation.
Even a small number of Campylobacter bacteria can cause infection — as few as 500 organisms can make a person sick.
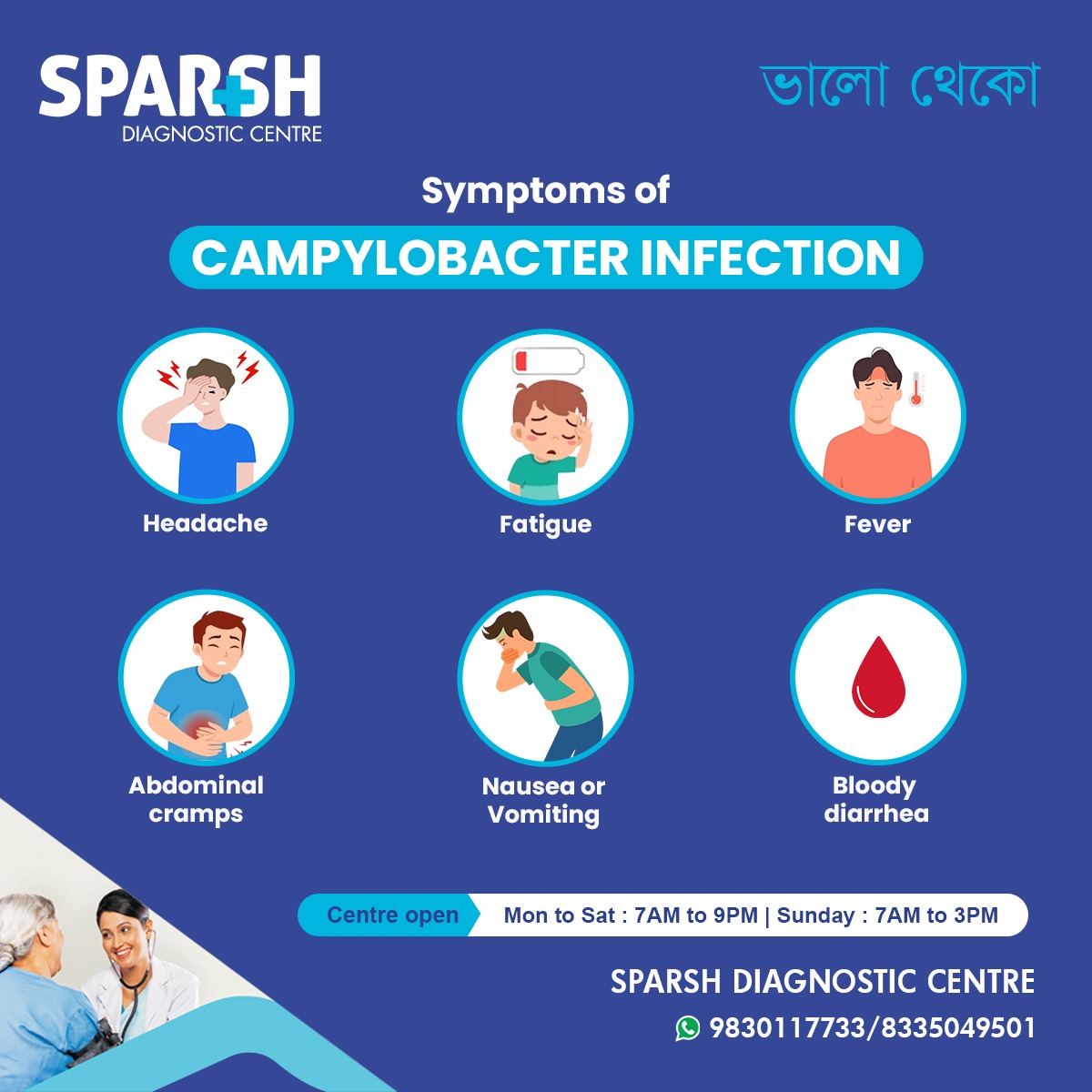
Symptoms of Campylobacter Infection
Symptoms usually appear 2 to 5 days after exposure. In most people, the illness lasts about a week. The infection can range from mild gastrointestinal upset to severe diarrhea with blood and mucus.
Common Symptoms Include:
Headache – Often one of the earliest signs, accompanied by general malaise.
Fatigue – Persistent tiredness and weakness due to dehydration and loss of nutrients.
Fever – A moderate to high fever (38–40°C) is typical during the infection’s early stages.
Abdominal cramps – Sharp, cramping pain in the lower abdomen, sometimes severe enough to mimic appendicitis.
Nausea or Vomiting – Common in more intense infections, leading to dehydration.
Bloody diarrhea – A hallmark symptom indicating intestinal inflammation caused by bacterial toxins.
Complications of Campylobacter Infection
While most infections resolve on their own, complications can develop in certain individuals, especially if left untreated.
Possible Complications Include:
Dehydration: Caused by excessive diarrhea and vomiting.
Bacteremia: When bacteria enter the bloodstream, leading to severe systemic infection.
Reactive arthritis: Joint pain and inflammation that can occur weeks after infection.
Guillain-Barré Syndrome (GBS): A rare neurological disorder that can develop following Campylobacter infection, leading to muscle weakness and paralysis.
Irritable Bowel Syndrome (IBS): Some patients develop chronic digestive problems even after recovery.
Who Is Most at Risk?
Certain groups are more susceptible to developing severe illness or complications from Campylobacter infection:
Infants and young children
Elderly individuals
Pregnant women
People with weakened immune systems (e.g., HIV/AIDS patients, transplant recipients)
Those who take antacids, which lower stomach acid that normally kills bacteria
Diagnosis of Campylobacter Infection
Accurate diagnosis is crucial for proper management and prevention of spread.
At Sparsh Diagnostic Centre, stool and culture tests are performed to confirm Campylobacter infection and rule out other bacterial causes.
Diagnostic Methods Include:
Stool Culture: The most common test, where stool samples are analyzed to detect Campylobacter jejuni or C. coli.
PCR (Polymerase Chain Reaction): Detects bacterial DNA, offering faster and more accurate results.
Blood Tests: In severe cases, to check for dehydration or systemic infection.
Early diagnosis helps guide treatment and prevent complications such as dehydration or GBS.
Treatment of Campylobacter Infection
Most Campylobacter infections resolve within 5 to 7 days without specific treatment. However, supportive care is essential to manage symptoms and prevent dehydration.
1. Hydration
The cornerstone of treatment is replacing lost fluids and electrolytes. Oral rehydration solutions (ORS) are recommended, especially for children and elderly patients.
2. Antibiotic Therapy
Antibiotics are prescribed in severe cases, prolonged illness, or when the patient is immunocompromised.
Commonly used antibiotics include:
Azithromycin
Erythromycin
Ciprofloxacin (used less due to rising resistance)
3. Rest and Nutrition
Patients are advised to rest and follow a bland diet (boiled rice, toast, bananas, applesauce) until symptoms improve. Dairy, caffeine, and spicy foods should be avoided during recovery.
4. Hospitalization
In severe dehydration, high fever, or bacteremia, hospitalization may be required for intravenous fluids and antibiotic administration.
Prevention of Campylobacter Infection
Preventive measures play a crucial role in reducing the risk of infection.
Food Safety Tips:
Cook poultry and meat thoroughly (internal temperature above 74°C).
Avoid consuming unpasteurized milk and untreated water.
Wash hands with soap after handling raw meat or pets.
Use separate cutting boards for raw and cooked foods.
Store foods at safe temperatures to prevent bacterial growth.
Wash fruits and vegetables properly before eating.
When Traveling:
Drink only bottled or boiled water.
Avoid ice cubes in drinks.
Eat freshly cooked, hot meals.
Campylobacter and Antibiotic Resistance
Antibiotic resistance among Campylobacter strains is a growing concern globally. Misuse and overuse of antibiotics in both humans and livestock contribute to resistance, making infections harder to treat.
To prevent antibiotic resistance:
Avoid self-medication.
Complete the full antibiotic course prescribed.
Maintain good hygiene and safe food practices.
When to See a Doctor
Seek medical attention immediately if you experience:
High fever (>39°C)
Persistent vomiting or inability to keep fluids down
Severe abdominal pain
Bloody diarrhea lasting more than 3 days
Signs of dehydration (dry mouth, sunken eyes, reduced urination)
If symptoms persist, diagnostic tests at Sparsh Diagnostic Centre can confirm infection and guide treatment.
Prognosis
Most individuals recover fully within a week with proper hydration and rest. However, complications like reactive arthritis or GBS may require longer medical follow-up. Preventing reinfection through hygiene and safe cooking habits is key to long-term health.
FAQs on Campylobacter Infection
1. What is the main cause of Campylobacter infection?
The infection is mainly caused by eating undercooked poultry or consuming contaminated food or water containing Campylobacter bacteria.
2. How long does Campylobacter infection last?
Most people recover within 5–7 days without specific treatment. However, symptoms like fatigue or bowel irregularities may persist for a few weeks.
3. Can Campylobacter infection be transmitted from person to person?
Direct person-to-person transmission is rare but possible, especially in settings with poor hygiene, such as childcare centers.
4. Is Campylobacter infection contagious?
Yes, the bacteria can spread through contaminated feces, food, or water, but good hygiene practices reduce the risk.
5. Can antibiotics help treat Campylobacter infection?
Yes, antibiotics like azithromycin or erythromycin may be prescribed in severe cases or for patients with weakened immune systems.
6. What foods are most likely to cause Campylobacter infection?
Undercooked chicken, unpasteurized milk, and contaminated water are common sources.
7. How can I prevent Campylobacter infection at home?
Ensure proper handwashing, cook poultry thoroughly, avoid cross-contamination in the kitchen, and only drink safe water.
8. Can Campylobacter infection cause long-term effects?
Rarely, it may cause Guillain-Barré Syndrome or chronic joint pain (reactive arthritis).
9. Is there a vaccine for Campylobacter infection?
Currently, there is no vaccine available. Prevention through hygiene and safe food handling is the best defense.
10. When should I visit a diagnostic centre?
If you experience severe diarrhea, dehydration, or prolonged symptoms, visit Sparsh Diagnostic Centre for stool testing and consultation.
Campylobacter infection may be common, but it’s largely preventable through safe food handling, clean water consumption, and good personal hygiene. Prompt diagnosis and treatment ensure a full recovery and prevent complications.
If you suspect a bacterial infection or are experiencing persistent gastrointestinal symptoms, visit Sparsh Diagnostic Centre for accurate testing and expert guidance.
Stay safe, eat well-cooked meals.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()






[…] by bacterial, viral, or parasitic infections. Bacteria such as E. coli, Salmonella, Shigella, and Campylobacter are common culprits, often contracted from contaminated food or […]
[…] Bacterial infections – E. coli, Salmonella, Campylobacter […]
[…] food or water or direct contact with an infected person. Other bacteria like Salmonella, Campylobacter, and certain strains of E. coli can also cause […]
[…] Campylobacter […]
[…] Campylobacter jejuni (a bacterial infection from contaminated food) […]
[…] Bacteria: Salmonella, E. coli, Listeria, Campylobacter […]