Leukopenia is a medical condition characterized by a reduced number of white blood cells (WBCs) in the blood. White blood cells are a vital part of the immune system, helping the body fight infections, bacteria, viruses, and other foreign invaders. When their levels drop below normal, the body becomes more vulnerable to infections, some of which can be severe or life-threatening if not detected early.
Leukopenia is not a disease in itself but rather a laboratory finding that often points toward an underlying condition. Understanding its causes, types, symptoms, and management is crucial for timely diagnosis and effective treatment.
What Is Leukopenia?
Leukopenia refers to a total white blood cell count lower than the normal range, which is typically:
Normal WBC count: 4,000 to 11,000 cells per microliter of blood
Leukopenia: WBC count less than 4,000 cells per microliter
White blood cells are produced in the bone marrow and circulate in the blood and lymphatic system. They include several subtypes, each with a specific role in immune defense. A reduction in any one or more of these cell types can lead to leukopenia.
Why Are White Blood Cells Important?
White blood cells protect the body by:
Identifying and destroying bacteria and viruses
Fighting fungal and parasitic infections
Removing damaged or abnormal cells
Supporting immune memory and long-term protection
When WBC levels fall, even minor infections can become serious, making early detection essential.
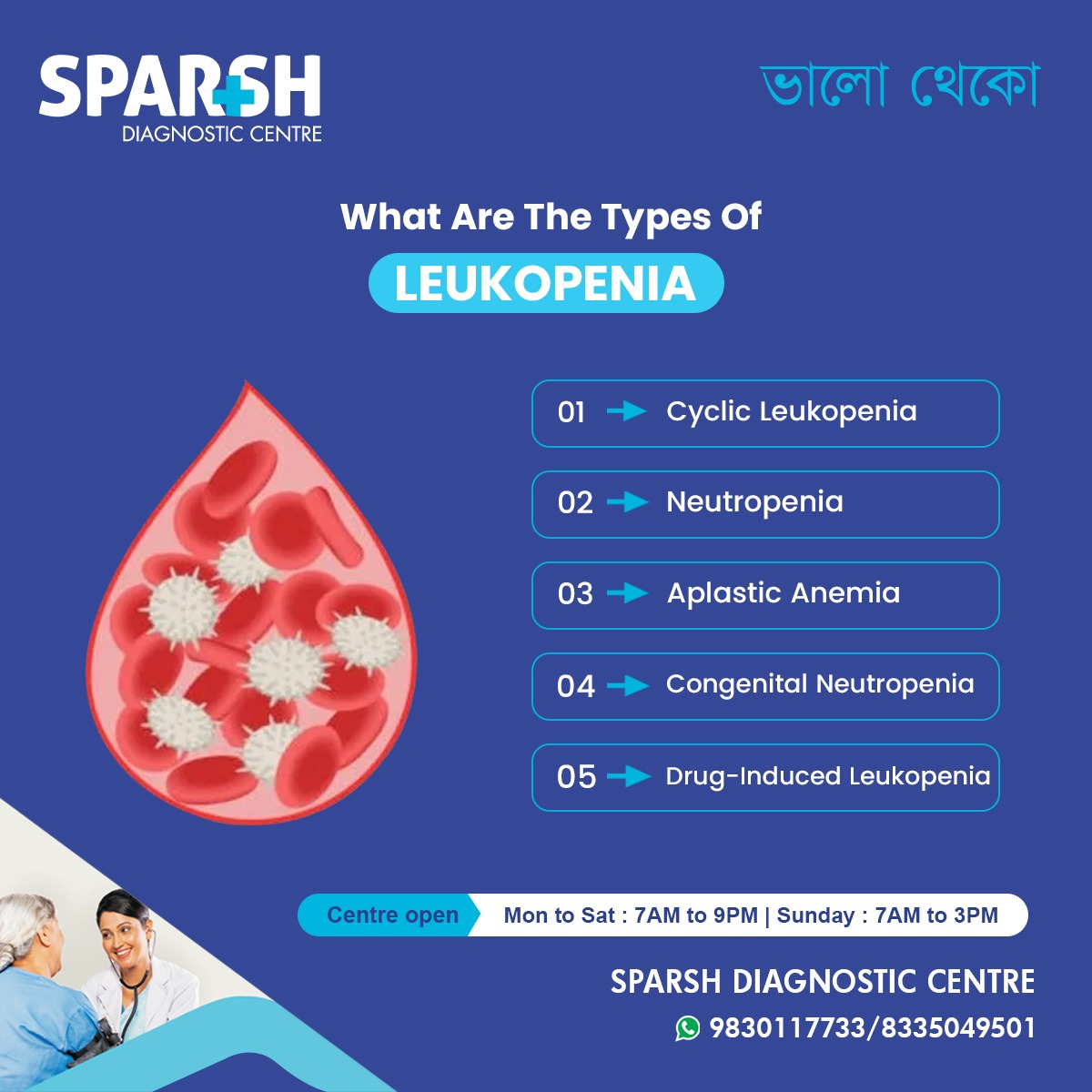
Types of Leukopenia
Leukopenia can be classified based on which type of white blood cell is reduced or how the condition develops.
1. Neutropenia
Neutropenia is the most common form of leukopenia and occurs when neutrophils, the primary infection-fighting cells, are low.
Causes include:
Viral infections
Chemotherapy or radiation therapy
Bone marrow disorders
Severe neutropenia significantly increases the risk of bacterial infections.
2. Lymphopenia (Lymphocytopenia)
This type involves a reduction in lymphocytes, which include T cells, B cells, and natural killer cells.
Common causes:
Long-term steroid use
Lymphopenia mainly affects the body’s ability to fight viral infections.
3. Cyclic Leukopenia
Cyclic leukopenia is a rare condition where WBC levels drop periodically, usually every 3–4 weeks, and then return to normal.
Key features:
Recurrent infections during low counts
Fever and mouth ulcers
Often genetic in origin
4. Congenital Neutropenia
This is a genetic disorder present from birth in which the bone marrow fails to produce enough neutrophils.
Children with this condition may experience:
Frequent infections
Delayed growth
Recurrent fevers
5. Drug-Induced Leukopenia
Certain medications can suppress bone marrow activity or destroy white blood cells.
Common drug groups involved:
Chemotherapy drugs
Anti-thyroid medications
Some antibiotics
Anti-epileptic drugs
In many cases, WBC counts recover after stopping the medication under medical supervision.
6. Leukopenia Due to Bone Marrow Disorders
Conditions that directly affect bone marrow function can reduce white blood cell production.
Examples include:
Aplastic anemia
Myelodysplastic syndromes
Causes of Leukopenia
Leukopenia can develop due to a wide range of conditions, including:
Infections
Autoimmune Disorders
Nutritional Deficiencies
Copper deficiency
Cancer and Cancer Treatment
Bone marrow cancers
Chemotherapy
Radiation therapy
Chronic Medical Conditions
Symptoms of Leukopenia
Leukopenia itself may not cause symptoms. However, symptoms usually arise from infections that occur due to low immunity.
Common symptoms include:
Frequent infections
Fever or chills
Recurrent respiratory infections
In severe cases, infections may spread rapidly and become life-threatening.
How Is Leukopenia Diagnosed?
1. Complete Blood Count (CBC)
A CBC test is the primary tool for diagnosing leukopenia. It measures:
Total white blood cell count
Differential count (types of WBCs)
2. Peripheral Blood Smear
This test examines blood cells under a microscope to assess their size, shape, and maturity.
3. Bone Marrow Examination
If the cause is unclear or a bone marrow disorder is suspected, a bone marrow biopsy may be recommended.
4. Additional Tests
Depending on suspected causes:
Vitamin B12 and folate levels
Viral markers
Autoimmune panels
Imaging studies
Treatment of Leukopenia
Treatment depends on the underlying cause and severity.
Treating the Root Cause
Managing infections with antibiotics, antivirals, or antifungals
Treating autoimmune diseases with immunosuppressants
Correcting nutritional deficiencies
Medications
Growth factors (G-CSF): Stimulate white blood cell production
Immunosuppressive therapy: In autoimmune cases
Lifestyle and Preventive Measures
Maintaining good hygiene
Avoiding crowded places during severe leukopenia
Eating a balanced, nutrient-rich diet
Regular medical follow-ups
Complications of Leukopenia
If untreated, leukopenia may lead to:
Severe or recurrent infections
Sepsis
Delayed recovery from illnesses
Increased hospitalization risk
Early diagnosis and regular monitoring significantly reduce complications.
Can Leukopenia Be Prevented?
Not all cases are preventable, but risk can be reduced by:
Regular health checkups
Balanced nutrition
Avoiding unnecessary medication use
Monitoring blood counts during chemotherapy or long-term drug therapy
When to See a Doctor?
Seek medical attention if you experience:
Persistent fever
Recurrent infections
Unexplained fatigue
Abnormal blood test results
Early evaluation can prevent serious outcomes.
Frequently Asked Questions (FAQs)
1. Is leukopenia dangerous?
Leukopenia can be serious if it leads to frequent or severe infections. The risk depends on how low the WBC count is and the underlying cause.
2. Can leukopenia be cured?
Leukopenia caused by infections or nutritional deficiencies is often reversible. Chronic or genetic causes may require long-term management.
3. What foods help increase white blood cells?
Foods rich in:
Vitamin B12 (eggs, dairy)
Folate (leafy greens)
Zinc (nuts, seeds)
Protein (lean meat, legumes)
support healthy immune function.
4. Is leukopenia the same as neutropenia?
No. Neutropenia is a type of leukopenia that specifically involves low neutrophils.
5. Can stress cause leukopenia?
Severe physical stress, infections, or chronic illness may contribute indirectly, but stress alone is not a common cause.
6. How often should WBC counts be monitored?
Monitoring depends on the cause. Patients undergoing chemotherapy or with chronic conditions may need frequent testing.
7. Can leukopenia affect children?
Yes. Leukopenia can occur in children due to infections, genetic disorders, or bone marrow conditions.
8. Does leukopenia always cause symptoms?
No. Mild leukopenia may be asymptomatic and detected only through routine blood tests.
Leukopenia is an important clinical finding that should never be ignored. While it may be temporary and mild in some cases, it can also signal serious underlying health issues. Early diagnosis through blood tests, identification of the root cause, and appropriate treatment are key to preventing complications.
Regular health checkups and expert diagnostic support play a crucial role in managing leukopenia effectively and safely.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

Sparsh Doctor List
![]()





[…] This leads to a condition known as cytopenia, which includes anemia (low red blood cells), leukopenia (low white blood cells), and thrombocytopenia (low platelets). Depending on which blood cell line is predominantly […]
[…] spleen destroys blood cells, leading to anemia, leukopenia, and […]
[…] Leukopenia (low white blood cell count) […]