Skin is the body’s largest organ, and any changes in its texture or appearance often reflect internal health conditions. One such skin disorder is Phrynoderma, also known as toad skin. This condition is primarily linked to nutritional deficiencies, particularly a lack of vitamin A, and presents as rough, raised bumps on the skin.
Although phrynoderma is not life-threatening, it is often an indicator of poor dietary intake, malnutrition, or underlying medical conditions that affect nutrient absorption. With proper diagnosis and treatment, this condition is reversible, making awareness and early intervention essential.
This article provides an in-depth look at phrynoderma, covering its causes, symptoms, risk factors, diagnosis, treatment, prevention, and frequently asked questions.
What is Phrynoderma?
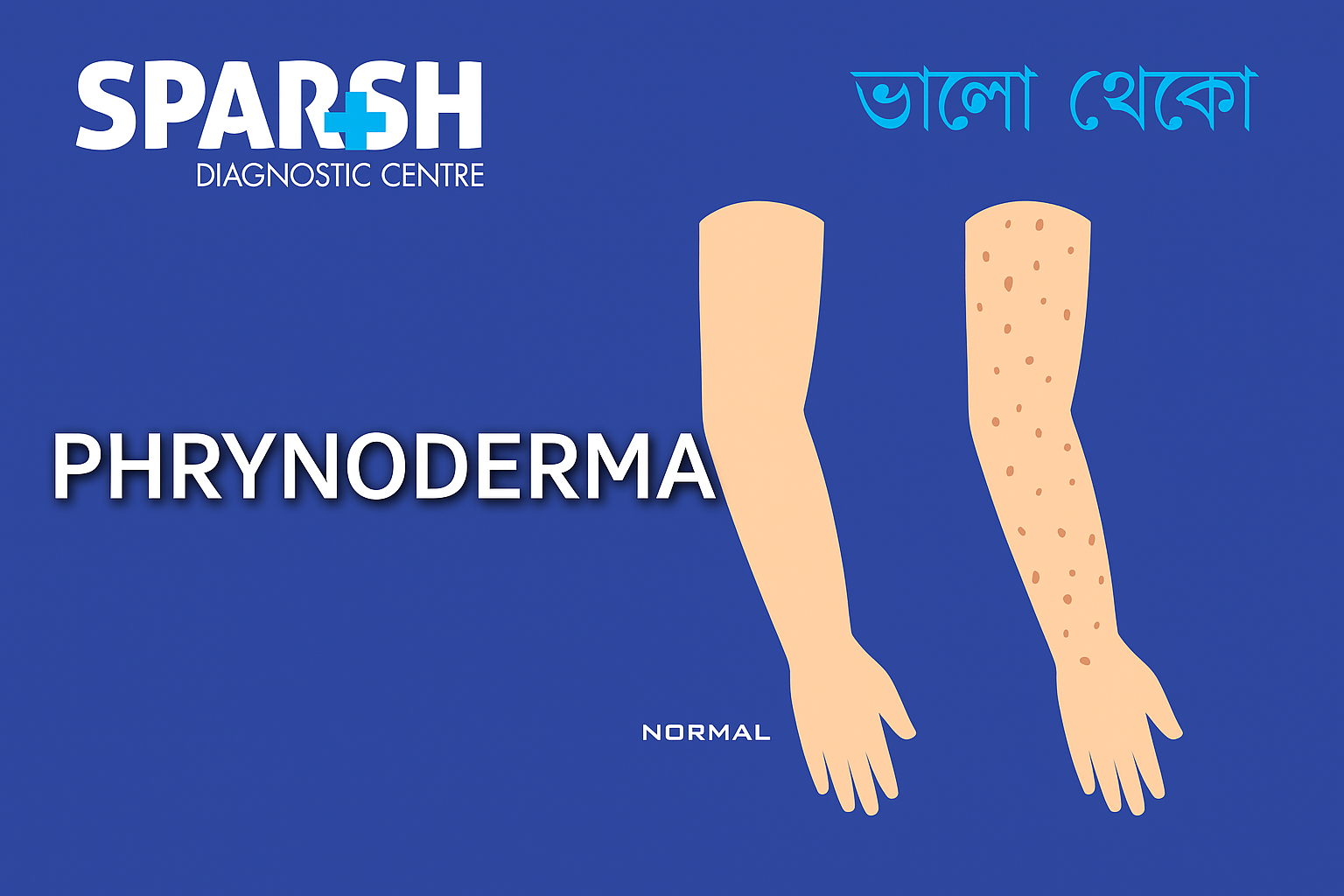
Phrynoderma is a form of follicular hyperkeratosis that occurs due to nutritional deficiencies, especially vitamin A deficiency. The name originates from the Greek word phrynos, meaning toad, because the skin develops a rough, bumpy texture resembling a toad’s skin.
This condition is commonly observed in children and young adults in developing countries, particularly where malnutrition and poor dietary diversity are prevalent.
Causes of Phrynoderma
The exact cause of phrynoderma is often multifactorial, but the primary contributors include:
1. Vitamin A Deficiency
The leading cause of phrynoderma.
Vitamin A is essential for healthy epithelial tissue and skin regeneration.
Deficiency leads to abnormal keratinization and follicular plugging.
2. Other Nutritional Deficiencies
Vitamin B complex deficiency (B2, B6, B12) contributes to skin changes.
Vitamin E deficiency worsens keratinization.
Essential fatty acid deficiency leads to dry, scaly skin.
Protein deficiency impairs skin repair and barrier function.
3. Malabsorption Disorders
Conditions like celiac disease, Crohn’s disease, chronic diarrhea, or pancreatic insufficiency reduce nutrient absorption, contributing to deficiencies.
4. Poor Diet and Malnutrition
A lack of fruits, vegetables, milk, eggs, and protein-rich foods increases the risk.
5. Other Contributing Factors
Chronic infections
Alcoholism
Poverty and limited access to balanced nutrition
Risk Factors for Phrynoderma
Some groups are more susceptible to developing this condition:
Children and adolescents with rapid growth demands.
Pregnant and lactating women, due to higher nutrient requirements.
People with chronic gastrointestinal diseases causing malabsorption.
Individuals with restricted diets, especially those lacking animal products.
Communities in low-income countries with high rates of malnutrition.
Symptoms of Phrynoderma
Phrynoderma primarily affects the skin and presents with the following features:
1. Skin Lesions
Small, rough, raised bumps resembling toad skin.
Usually appear on the extensor surfaces of arms, thighs, buttocks, and sometimes face.
Follicles may be plugged with keratin.
2. Texture and Appearance
Skin feels coarse and rough to touch.
Bumps may merge into larger patches.
Dryness and scaling are common.
3. Associated Symptoms
Night blindness or poor vision in dim light (due to vitamin A deficiency).
Dry eyes (xerophthalmia).
Brittle hair and nails.
Fatigue, irritability, or weakness if multiple deficiencies coexist.
Complications of Phrynoderma
If untreated, phrynoderma may lead to:
Persistent rough, unattractive skin.
Severe vitamin A deficiency complications, including blindness.
Increased susceptibility to infections due to poor skin barrier.
Poor growth and development in children.
Long-term malnutrition effects such as anemia and weakened immunity.
Diagnosis of Phrynoderma
Diagnosis is primarily clinical but may require additional investigations.
Clinical Examination
Dermatologists identify follicular hyperkeratotic papules on arms, thighs, and buttocks.
Toad-skin texture is a classic sign.
Medical History
Dietary assessment (low intake of vitamin A, protein, or fats).
History of gastrointestinal disorders or chronic illness.
Laboratory Tests
Serum vitamin A levels
Other vitamin and mineral levels
Complete blood count (to check for anemia)
Liver function tests (important as vitamin A is stored in the liver)
Treatment of Phrynoderma
The cornerstone of treatment is nutritional correction and supportive skin care.
1. Nutritional Supplementation
Vitamin A supplementation: Oral capsules or injections (as prescribed).
B-complex vitamins: Riboflavin, pyridoxine, and cyanocobalamin.
Vitamin E supplementation.
Essential fatty acids: Found in vegetable oils, nuts, and seeds.
Protein-rich foods: Eggs, fish, milk, legumes, and meat.
2. Dietary Modifications
Increase intake of vitamin A-rich foods: carrots, spinach, kale, sweet potatoes, mangoes, papaya.
Include milk, butter, eggs, and liver in diet.
Add nuts, seeds, and vegetable oils for essential fatty acids.
Maintain a balanced diet with adequate protein.
3. Skin Care
Use moisturizing creams to reduce dryness.
Gentle exfoliation to improve skin texture.
Avoid harsh soaps that worsen dryness.
4. Treating Underlying Conditions
Manage gastrointestinal disorders that cause malabsorption.
Address alcoholism or chronic infections if present.
Prevention of Phrynoderma
Prevention focuses on ensuring a well-balanced diet and addressing risk factors:
Regular intake of vitamin A-rich foods.
Public health programs promoting supplementation in high-risk populations.
Awareness campaigns in rural and low-income areas.
Early detection and treatment of malabsorption syndromes.
Nutritional counseling during pregnancy and childhood.
Living with Phrynoderma
The condition is reversible with proper treatment. Once vitamin and nutrient levels are restored, skin texture improves significantly.
Children often show rapid improvement after supplementation.
Consistent healthy eating habits prevent recurrence.
Dermatologists may recommend periodic check-ups for those with chronic health issues.
Frequently Asked Questions (FAQ) about Phrynoderma
1. What is the main cause of phrynoderma?
The primary cause is vitamin A deficiency, though deficiencies in vitamin B complex, vitamin E, essential fatty acids, and proteins also contribute.
2. What does phrynoderma look like?
It appears as rough, raised, toad-like bumps on the skin, commonly on the arms, thighs, and buttocks.
3. Can phrynoderma be cured?
Yes, phrynoderma is reversible with proper nutritional supplementation and a balanced diet.
4. Who is most at risk of phrynoderma?
Children, adolescents, pregnant women, and people with malnutrition or gastrointestinal diseases are at higher risk.
5. Can phrynoderma cause blindness?
If due to severe vitamin A deficiency, phrynoderma may be accompanied by night blindness or other eye problems, which can progress to blindness if untreated.
6. How is phrynoderma diagnosed?
It is diagnosed clinically by dermatologists and confirmed with dietary history and blood tests for vitamin levels.
7. What foods help prevent phrynoderma?
Carrots, spinach, sweet potatoes, papaya, mangoes, eggs, milk, fish, liver, nuts, and seeds are excellent preventive foods.
8. Is phrynoderma contagious?
No, it is not an infectious disease. It results from nutritional deficiencies and cannot spread from person to person.
Phrynoderma is a skin condition caused mainly by nutritional deficiencies, especially vitamin A deficiency. While its toad-like skin appearance can cause cosmetic concerns, it is also a vital indicator of underlying malnutrition. Early detection and treatment with proper nutrition, supplementation, and skin care can reverse the condition and prevent complications.
Public health awareness, dietary education, and supplementation programs play a key role in eradicating phrynoderma, especially in vulnerable populations. By maintaining a balanced diet rich in vitamins, proteins, and essential fatty acids, phrynoderma can be prevented and effectively managed.
To consult a Dermatologist at Sparsh Diagnostic Centre, call our helpline number 9830117733.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()