Have you ever felt dizzy or faint when standing up suddenly? This could be more than just a fleeting moment of lightheadedness — it might be a sign of orthostatic hypotension. Also known as postural hypotension, this condition can significantly affect your daily life if not addressed properly.
In this in-depth guide from Sparsh Diagnostic Centre, we explain everything you need to know about orthostatic hypotension — from its causes and types to how it is diagnosed and treated.
What is Orthostatic Hypotension?
Orthostatic hypotension is a form of low blood pressure (hypotension) that occurs when you stand up from sitting or lying down. It’s typically defined as a drop in systolic blood pressure of 20 mm Hg or more, or diastolic blood pressure of 10 mm Hg or more within three minutes of standing.
This sudden drop can reduce blood flow to the brain, resulting in symptoms like dizziness, blurred vision, weakness, and even fainting.
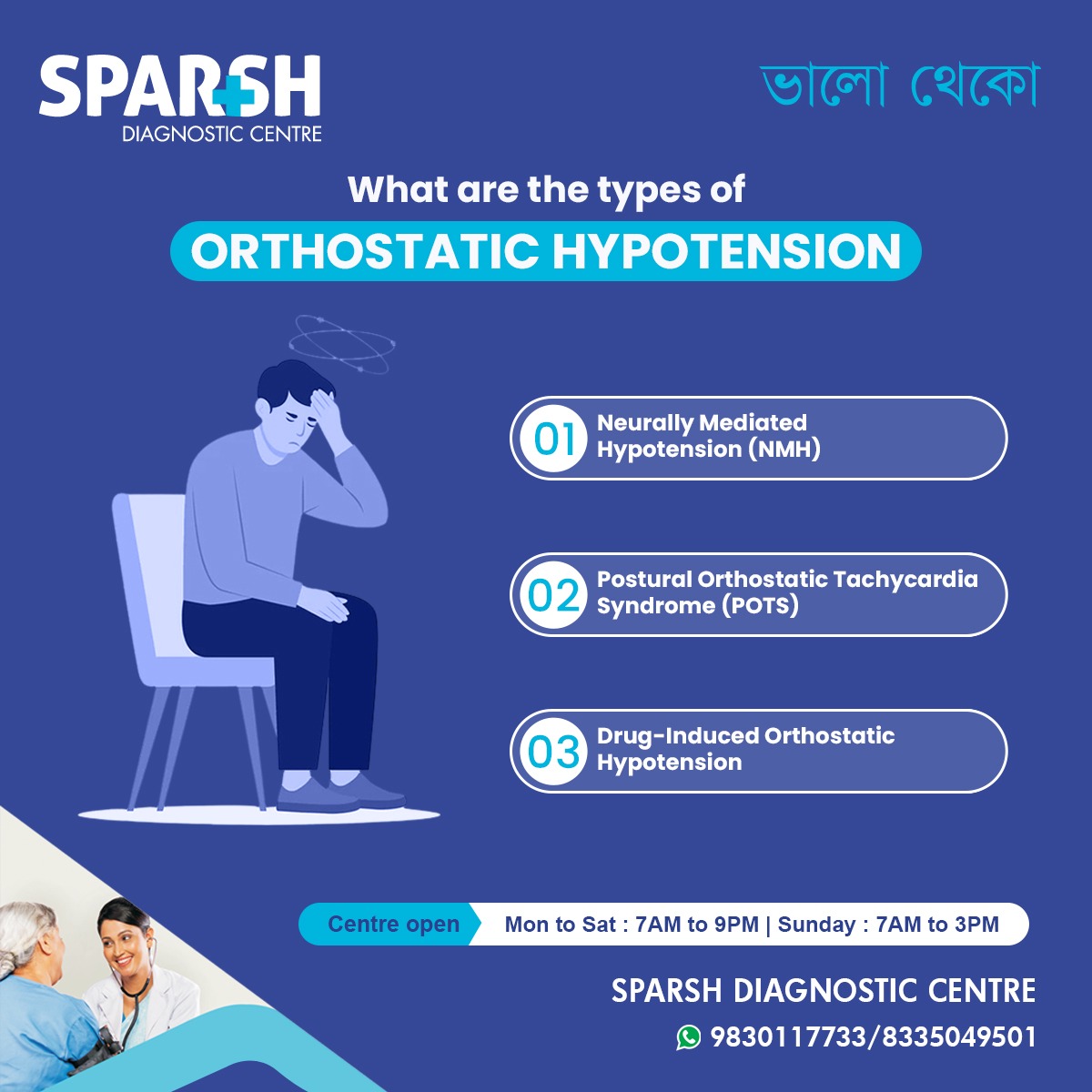
Types of Orthostatic Hypotension
Based on clinical presentations and causes, orthostatic hypotension can be classified into the following types:
1. Neurally Mediated Hypotension (NMH)
Also known as neurocardiogenic syncope, NMH occurs when the nervous system misinterprets signals from the heart and blood vessels, causing a drop in blood pressure and heart rate. It is more common in children and young adults.
Symptoms:
Lightheadedness
Sweating
2. Postural Orthostatic Tachycardia Syndrome (POTS)
POTS is a condition characterized by a rapid increase in heart rate (more than 30 beats per minute) within 10 minutes of standing, without a significant drop in blood pressure.
It often affects young women and may be associated with fatigue, brain fog, and palpitations.
Symptoms:
Dizziness
Fast heartbeat
Chest discomfort
Difficulty concentrating
3. Drug-Induced Orthostatic Hypotension
Certain medications can lower blood pressure too much, especially in elderly patients, leading to postural drops in blood pressure. Common culprits include:
Diuretics
Alpha-blockers
Beta-blockers
Antidepressants
Parkinson’s medications
Symptoms:
Lightheadedness when standing
Weakness
Falls
Visual disturbances
Other Classifications
Orthostatic hypotension may also be categorized based on its underlying cause:
Primary autonomic failure (e.g., Parkinson’s disease, multiple system atrophy)
Secondary autonomic failure (e.g., diabetes, amyloidosis)
Non-neurogenic causes (e.g., dehydration, blood loss)
What Causes Orthostatic Hypotension?
The body usually compensates for gravity by narrowing blood vessels and increasing heart rate when you stand. However, in orthostatic hypotension, these mechanisms fail to activate effectively.
Common Causes Include:
Heart problems (e.g., heart failure, bradycardia)
Endocrine disorders (e.g., Addison’s disease, diabetes)
Nervous system disorders
Prolonged bed rest or immobility
Medications
Blood loss or anemia
Signs and Symptoms of Orthostatic Hypotension
Some people may be asymptomatic, while others experience noticeable symptoms, especially when changing position.
Common Symptoms:
Dizziness or lightheadedness
Blurred or tunnel vision
Weakness
Fainting (syncope)
Nausea
Confusion
Fatigue
Head and neck pain (especially in the back of the head)
These symptoms typically occur within seconds to minutes of standing and usually improve when sitting or lying down.
Who Is at Risk?
Orthostatic hypotension can affect people of all ages, but some groups are at higher risk:
Elderly (age-related changes in blood pressure regulation)
People with diabetes
Patients with Parkinson’s or other neurodegenerative diseases
Individuals taking blood pressure-lowering medications
Pregnant women
Those with chronic dehydration or anemia
How is Orthostatic Hypotension Diagnosed?
Accurate diagnosis involves clinical evaluation, medical history, and specific diagnostic tests.
1. Blood Pressure Monitoring
BP is measured while lying down, then after 1 and 3 minutes of standing.
A drop of ≥20 mm Hg systolic or ≥10 mm Hg diastolic confirms the diagnosis.
2. Tilt Table Test
The patient is strapped to a motorized table that tilts to simulate standing.
Used to evaluate unexplained fainting or differentiate between POTS and NMH.
3. Electrocardiogram (ECG)
Detects arrhythmias or other heart abnormalities.
4. Blood Tests
To identify anemia, blood sugar levels, or hormonal imbalances.
5. Echocardiogram
To assess heart function and rule out structural heart disease.
6. Autonomic Function Tests
Evaluate the nervous system’s ability to regulate blood pressure.
Complications of Orthostatic Hypotension
If left untreated, orthostatic hypotension can lead to:
Falls and fractures
Frequent fainting
Reduced quality of life
Increased risk of cardiovascular events
Cognitive dysfunction in the elderly
Treatment and Management
Management depends on the underlying cause, severity, and patient’s age and medical condition.
1. Lifestyle Modifications
Increase salt and fluid intake (if not contraindicated)
Rise slowly from sitting or lying positions
Wear compression stockings
Elevate the head of the bed
Eat small, frequent meals
2. Physical Counterpressure Maneuvers
Techniques like:
Leg crossing
Squatting
Abdominal tensing
These help push blood back to the heart when standing.
3. Medication Adjustment
Reduce or stop offending drugs.
Change dosing time (e.g., take antihypertensives at bedtime).
4. Pharmacological Therapy
If lifestyle changes aren’t enough:
Fludrocortisone: Increases blood volume.
Midodrine: Constricts blood vessels to raise BP.
Pyridostigmine: Enhances neurotransmitter signaling.
Droxidopa: For neurogenic orthostatic hypotension.
Always consult a healthcare provider before starting any medication.
Prevention Tips
To reduce your risk or prevent recurrence of orthostatic hypotension:
Stay hydrated, especially during hot weather.
Avoid prolonged standing or rapid changes in posture.
Be cautious with medications that may lower blood pressure.
Monitor blood pressure regularly, especially if you’re older or diabetic.
Exercise regularly to improve circulation and cardiovascular health.
Orthostatic Hypotension in Special Populations
In Elderly
Common due to impaired autonomic regulation.
Increases risk of falls and cognitive issues.
In Diabetics
Often due to autonomic neuropathy.
Blood sugar control is essential.
During Pregnancy
Normal due to hormonal changes and vascular relaxation.
Usually improves postpartum.
When to See a Doctor
You should consult a healthcare provider if you:
Feel faint or dizzy often when standing.
Have unexplained falls or blackouts.
Are taking medications and suspect they may be causing symptoms.
Are managing chronic conditions like diabetes, Parkinson’s, or hypertension.
Early diagnosis and management can prevent complications and improve quality of life.
Orthostatic hypotension may seem like a simple drop in blood pressure, but it can be a sign of an underlying issue and may significantly impair daily functioning. With the right diagnosis, lifestyle modifications, and treatment, most people can effectively manage their symptoms.
If you or a loved one are experiencing symptoms, visit Sparsh Diagnostic Centre for a thorough evaluation and personalized care. Our expert physicians and modern diagnostic facilities are equipped to help you stay on your feet — safely.
Sparsh Diagnostic Centre — Your Partner in Holistic Healthcare
📍 Centre Open:
Monday to Saturday – 7 AM to 9 PM
Sunday – 7 AM to 3 PM
📞 Contact:
9830117733 / 8335049501
Stay informed. Stay upright. Stay healthy.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()






[…] pressure fluctuations (orthostatic hypotension or […]
[…] Orthostatic Hypotension:A sudden drop in blood pressure when standing up, causing dizziness, lightheadedness, or even fainting (syncope). […]
[…] Orthostatic Hypotension […]
[…] Orthostatic hypotension: Occurs when a person stands up too quickly, causing a sudden drop in blood pressure and leading to fainting. […]
[…] ABPM assists in differentiating between true hypertension and orthostatic hypotension (BP drop on standing). […]
[…] Classic Orthostatic Hypotension – Low blood pressure after standing, but without the abnormal nerve reflex seen in NMH. […]
[…] Orthostatic Hypotension […]
[…] Orthostatic hypotension (drop in BP when standing) […]
[…] Orthostatic Hypotension: Sudden drops in blood pressure when standing, causing dizziness or fainting […]
[…] Orthostatic Hypotension: A sudden drop in blood pressure when standing up from a sitting or lying position. This can cause dizziness or lightheadedness. […]