Avascular necrosis (AVN) of the hip, also known as osteonecrosis, is a serious orthopedic condition where the blood supply to the femoral head (the ball of the hip joint) is disrupted, leading to the death of bone tissue. If untreated, it can cause the bone to collapse, resulting in severe pain, arthritis, and the eventual need for hip replacement surgery.
This comprehensive blog explores the causes, risk factors, symptoms, diagnosis, and treatment options for avascular necrosis of the hip, and emphasizes the importance of early intervention for better outcomes.
What Is Avascular Necrosis of the Hip?
Avascular necrosis (AVN) literally means “death of bone tissue due to lack of blood supply.” The hip joint is particularly susceptible because the femoral head relies on a limited and delicate blood supply. When this supply is impaired or cut off, bone tissue begins to die, leading to joint destruction over time.
Causes of Avascular Necrosis of the Hip
AVN can result from various underlying conditions or factors that interfere with blood circulation to the femoral head:
1. Trauma
Injury to the hip, such as a fracture or dislocation, can damage the blood vessels supplying the femoral head. This is one of the most common causes of AVN.
2. Long-term Steroid Use
High-dose corticosteroids like prednisone, when used over extended periods, are associated with AVN. The exact mechanism isn’t fully understood, but steroids may increase fat levels in the blood, clogging small blood vessels.
3. Excessive Alcohol Consumption
Heavy alcohol intake can lead to fat buildup in blood vessels, reducing blood flow to the bone.
4. Medical Conditions
Decompression sickness (in divers)
5. Radiation and Chemotherapy
Treatment for cancers involving the pelvis or hips can damage bone tissue or its blood supply, increasing the risk of AVN.
6. Idiopathic AVN
In some cases, the exact cause remains unknown, and this is referred to as idiopathic AVN.
Who Is at Risk?
Certain individuals are at higher risk of developing AVN of the hip:
People aged 30 to 50 years
Those with a history of hip injury or dislocation
Patients on long-term corticosteroid therapy
Individuals with alcohol dependency
Patients with autoimmune diseases like lupus
People undergoing organ transplants
Signs and Symptoms
AVN typically progresses through stages, with symptoms evolving over time.
Early Stages:
Mild or no pain
Discomfort with activity, especially walking or running
Intermediate Stages:
Persistent hip or groin pain
Pain that worsens with weight-bearing
Reduced hip mobility
Limping
Advanced Stages:
Severe, constant pain
Loss of joint function
Collapse of the femoral head
Development of osteoarthritis
The pain often radiates from the groin to the thigh or buttock and may increase during activities like climbing stairs or prolonged standing.
How Is Avascular Necrosis Diagnosed?
Early diagnosis is key to preserving the hip joint. Your doctor may recommend the following tests:
1. Physical Examination
Checking for pain, range of motion, and limping
Identifying tender areas around the hip
2. Imaging Tests
X-rays: May appear normal in early AVN but show bone collapse in later stages.
MRI: The most sensitive test for early AVN; detects bone marrow changes before visible damage.
CT scan: Helps assess the extent of bone damage.
Bone scan: Identifies changes in bone metabolism.
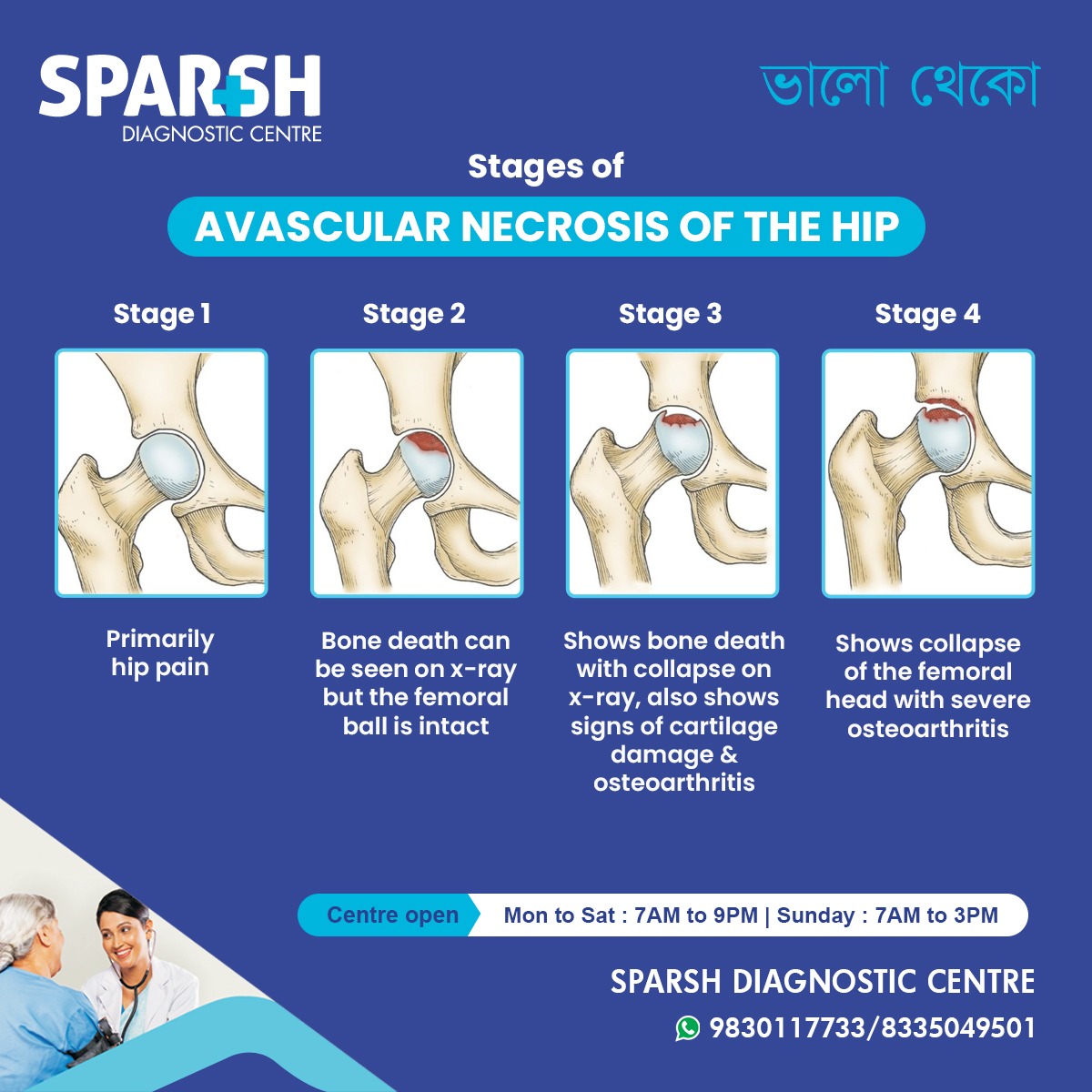
Stages of Avascular Necrosis of the Hip
AVN is typically classified using the Ficat and Arlet classification system, which has four stages:
Stage I: Normal X-ray, early changes on MRI
Stage II: Sclerosis or cyst formation visible on X-ray, no collapse
Stage III: Subchondral fracture (“crescent sign”), early collapse of the femoral head
Stage IV: Advanced collapse with joint space narrowing and arthritis
Treatment Options
Treatment for AVN depends on the stage, severity, and cause. The goal is to relieve pain, preserve the femoral head, and restore mobility.
1. Non-Surgical Treatments (Early Stages)
a. Medications
NSAIDs: To relieve pain and inflammation
Bisphosphonates: May slow bone damage
Blood thinners: If clotting is a concern
b. Physical Therapy
Focused on improving range of motion
Low-impact exercises like swimming or cycling
c. Activity Modification
Limiting weight-bearing activities using crutches or a walker
Avoiding high-impact sports
d. Electrical Stimulation
Promotes bone growth and healing using low-level electrical currents
2. Surgical Treatments
a. Core Decompression
A surgical drill is used to remove a part of the inner bone, reducing pressure and creating space for new blood vessels. Best for early-stage AVN.
b. Bone Grafting
Healthy bone tissue (either from the patient or donor) is grafted to support regeneration. May be used alongside core decompression.
c. Osteotomy
The femur is cut and realigned to shift weight off the damaged area of the femoral head. This preserves the joint but is technically complex.
d. Total Hip Replacement (THR)
Also known as hip arthroplasty, this is the most effective option for advanced AVN. The damaged femoral head is replaced with a prosthetic.
e. Stem Cell Therapy
Still under research, this involves injecting stem cells into the necrotic area to promote bone healing.
Preventing Avascular Necrosis of the Hip
While not all causes are preventable, you can lower your risk by:
Avoiding excessive alcohol
Using steroids only when necessary and under medical supervision
Managing underlying health conditions like diabetes or sickle cell disease
Protecting your hips during high-risk activities
Regular check-ups if you are on long-term medication that may affect bone health
Complications of Untreated AVN
If left untreated, AVN can lead to:
Collapse of the femoral head
Osteoarthritis
Chronic hip pain
Severe mobility loss
Need for major joint replacement surgery
Prompt diagnosis and treatment can significantly improve outcomes.
Living with Avascular Necrosis of the Hip
Coping with AVN involves a multidisciplinary approach. Patients may need support from orthopedic surgeons, physical therapists, and pain management specialists.
Tips for Daily Life:
Use mobility aids like canes or crutches when needed
Maintain a healthy weight to reduce stress on joints
Engage in low-impact exercises like yoga or swimming
Monitor pain levels and consult your doctor regularly
Prognosis and Recovery
With early treatment, many patients can avoid surgery and maintain a high quality of life. However, once the femoral head collapses, hip replacement becomes the definitive treatment. Fortunately, modern surgical techniques offer excellent long-term results, with most patients regaining mobility and pain relief.
Recovery times vary depending on the treatment:
Core decompression: 3–6 months
Hip replacement: 6–12 weeks for most daily activities
When to See a Doctor
Seek medical advice if you experience:
Persistent or worsening hip or groin pain
Difficulty walking or bearing weight
Hip pain that doesn’t improve with rest
Early evaluation by an orthopedic specialist can prevent irreversible damage.
Avascular necrosis of the hip is a progressive and potentially debilitating condition that requires early intervention. Recognizing the symptoms, understanding your risk factors, and seeking prompt medical attention can help preserve your hip joint and avoid major surgery. With modern diagnostic tools and advanced treatment options, living an active, pain-free life with AVN is possible.
If you’re experiencing hip pain or have risk factors like steroid use or alcohol dependence, consult your healthcare provider or orthopedic specialist for a timely evaluation.
Need an Expert Diagnosis or Imaging Test?
Visit Sparsh Diagnostic Centre for advanced imaging services and orthopedic consultations.
Stay mobile. Stay pain-free. Stay healthy.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()