Kidney failure, also known as end-stage renal disease (ESRD), is a life-threatening condition where the kidneys lose their ability to filter waste and maintain fluid and electrolyte balance. When this happens, two major treatment options are available to patients: dialysis or a kidney transplant.
Each of these life-sustaining therapies comes with its own benefits, challenges, and long-term implications. Making an informed decision between kidney transplant and dialysis requires understanding the differences in survival rates, quality of life, complications, and costs associated with each.
This blog explores both treatment options in detail to help patients, families, and caregivers make the best choice based on medical condition, lifestyle, and personal preferences.
Understanding the Basics
What Is Dialysis?
Dialysis is a medical procedure that replicates some functions of a healthy kidney. It removes waste, toxins, and excess fluid from the blood when the kidneys can no longer perform these essential tasks.
There are two main types of dialysis:
Hemodialysis (HD): Blood is filtered using a dialysis machine.
Peritoneal Dialysis (PD): Fluid is introduced into the abdomen to absorb waste, which is later drained.
Most patients undergo dialysis multiple times per week, with each session lasting 3–5 hours.
What Is a Kidney Transplant?
A kidney transplant involves surgically placing a healthy kidney from a donor into a patient with kidney failure. The new kidney takes over the function of the failed organs, offering a more permanent and physiological solution compared to dialysis.
Donor kidneys can be:
Living donor kidneys (from a family member or friend).
Deceased donor kidneys (from brain-dead or recently deceased donors).
Quality of Life: Kidney Transplant vs Dialysis
Dialysis and Its Impact on Daily Life
Dialysis can be physically and emotionally exhausting. Since it requires multiple sessions every week, it often disrupts work, travel, and daily routines. Common complaints from dialysis patients include:
Fatigue after sessions
Fluid and dietary restrictions
Risk of infections (especially for peritoneal dialysis)
Needle pain or fistula complications (for hemodialysis)
Over time, many patients on long-term dialysis experience a decline in physical and mental health.
Kidney Transplant: A Return to Normalcy
In contrast, a successful kidney transplant can dramatically improve a patient’s quality of life. Benefits include:
Freedom from dialysis
Less restrictive diet and fluid intake
Improved energy and physical activity levels
Better psychological well-being
Many transplant recipients are able to return to work, travel, exercise, and enjoy a lifestyle that closely resembles life before kidney failure.
Survival Rates and Long-Term Outcomes
Dialysis: A Lifesaving But Limited Option
Dialysis can sustain life for many years, but long-term survival is lower compared to transplantation. According to global data:
The 5-year survival rate for patients on dialysis ranges from 30% to 50%.
Dialysis patients are at higher risk for cardiovascular disease, infections, and other complications.
Kidney Transplant: Better Survival Rates
Kidney transplants generally offer better long-term survival. Statistics show:
The 5-year survival rate post-transplant is over 85% for deceased donor kidneys and over 90% for living donor kidneys.
Transplanted kidneys from living donors can function for 15–20 years or more.
Hence, for suitable candidates, transplantation provides a significantly better prognosis.
Complications and Side Effects
Complications with Dialysis
Though dialysis is lifesaving, it carries multiple risks:
Infection: Especially for peritoneal dialysis or from dialysis access sites.
Heart and vascular issues: Dialysis increases the risk of cardiovascular disease.
Low blood pressure, muscle cramps, and fatigue post-dialysis.
Bone disease and anemia from long-term use.
Complications with Transplants
While kidney transplants avoid dialysis-related complications, they come with their own risks:
Rejection of the new kidney: Requires lifelong immunosuppressants to prevent this.
Infections: Immunosuppressants weaken the immune system.
Cancer risk: Slightly higher due to chronic immune suppression.
Side effects of immunosuppressive drugs: Can include high blood pressure, diabetes, or bone thinning.
Despite these risks, the overall health burden is often lower in transplant patients compared to those on dialysis.
Cost Comparison: Short-Term vs Long-Term
Dialysis: Ongoing and Expensive
Dialysis costs accumulate over time. Patients must pay for:
Frequent sessions (often 3x per week)
Medications (e.g., erythropoietin, phosphate binders)
Hospital visits for complications
Travel expenses to and from dialysis centers
According to studies, dialysis becomes more expensive than transplant after 2–3 years.
Transplant: High Initial Cost, Lower Long-Term Cost
Kidney transplantation involves high initial costs, including:
Surgery
Hospital stay
Diagnostic tests
Immunosuppressive medications
However, in the long term, transplant patients often incur fewer costs due to:
No need for dialysis
Fewer hospital admissions
Reduced need for ongoing medications (beyond immunosuppressants)
In the long run, transplantation is often more cost-effective.
Accessibility and Availability
Challenges with Dialysis
While dialysis centers are available in many urban and semi-urban locations, access can be limited in rural areas. Travel burden, scheduling issues, and machine availability can be limiting factors.
Challenges with Kidney Transplants
Donor availability is a major bottleneck. Thousands of patients are on transplant waiting lists.
Legal and ethical considerations surrounding organ donation can delay transplants.
Matching blood type and tissue compatibility also affect eligibility.
Despite these challenges, living donor transplantation can speed up the process and provide better outcomes.
Lifelong Considerations
Dialysis Requires Lifelong Commitment
Unless a transplant is performed, dialysis becomes a lifelong treatment. Patients must adjust their lifestyle around dialysis schedules, fluid intake, and dietary limits.
Transplant Requires Lifelong Immunosuppression
While transplantation offers freedom from dialysis, it requires lifelong immunosuppressive therapy to prevent organ rejection. Regular follow-up and monitoring are also necessary.
Suitability: Who Can Get a Transplant?
Not all dialysis patients are eligible for a transplant. Suitability depends on:
Age and overall health
Presence of comorbidities like cancer, severe heart disease, or infections
Psychological readiness and ability to adhere to medication regimens
Younger, healthier patients with good support systems tend to be better transplant candidates.
Patient Preferences and Psychological Aspects
Dialysis: Known Routine, Predictable
Some patients prefer the predictability and routine of dialysis, especially if they fear surgery or organ rejection. Older adults or those with multiple health issues may opt to continue dialysis rather than face the risks of surgery.
Transplant: A New Lease on Life
Others view transplant as a path to freedom—freedom from machines, needles, and hospital visits. Most patients report higher satisfaction post-transplant, citing greater independence and improved mental health.
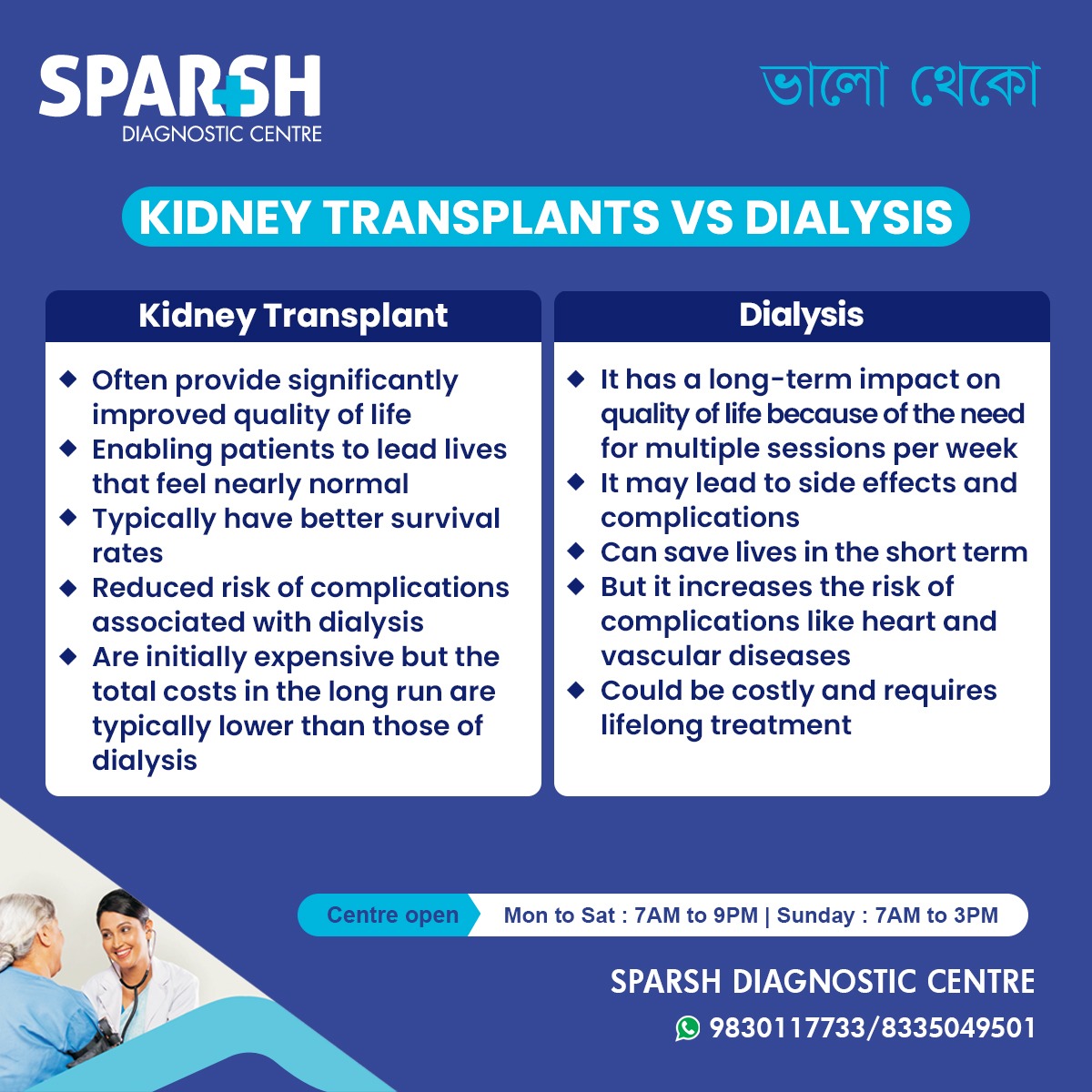
Key Takeaways: Kidney Transplant vs Dialysis
| Feature | Kidney Transplant | Dialysis |
|---|---|---|
| Quality of Life | Significantly improved | Limited due to frequent sessions |
| Survival Rates | Higher long-term survival | Lower long-term survival |
| Complications | Lower in long run | High risk of heart disease and infections |
| Cost | High upfront, lower long-term | Ongoing high expenses |
| Lifestyle Impact | Freedom from machines | Regular hospital visits and dietary limits |
| Accessibility | Dependent on donor availability | Widely available but logistically demanding |
When Should You Consider a Kidney Transplant?
Kidney transplant is usually recommended for:
ESRD patients with no contraindications
Patients under 70 with good heart function
Those able to comply with lifelong medications
Patients with a living donor available
Your nephrologist will assess whether you’re a good candidate.
Final Verdict: Which One Is Right for You?
Choosing between kidney transplant and dialysis is a deeply personal decision influenced by medical eligibility, lifestyle goals, and emotional readiness.
For many, a kidney transplant offers a better quality of life and long-term survival.
Dialysis is still a vital life-saving bridge, especially for those awaiting transplants or not eligible for surgery.
Consulting a nephrologist and transplant specialist is crucial. They can help weigh the pros and cons specific to your condition and guide you through the next steps.
Whether you choose dialysis or transplantation, the journey of managing kidney failure is one that demands support, education, and medical supervision. Advances in both fields have significantly improved outcomes, giving hope and life to millions.
If you or a loved one is facing end-stage kidney disease, reach out to a trusted healthcare provider like Sparsh Diagnostic Centre. Our expert team can help you navigate diagnosis, dialysis, transplant eligibility, and post-treatment care with compassion and precision.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()






[…] Over time, this leads to protein leakage in urine (proteinuria), increased blood pressure, swelling (edema), and eventually chronic kidney disease (CKD) or end-stage renal disease (ESRD) requiring dialysis or kidney transplant. […]
[…] In severe cases, dialysis or kidney transplant. […]