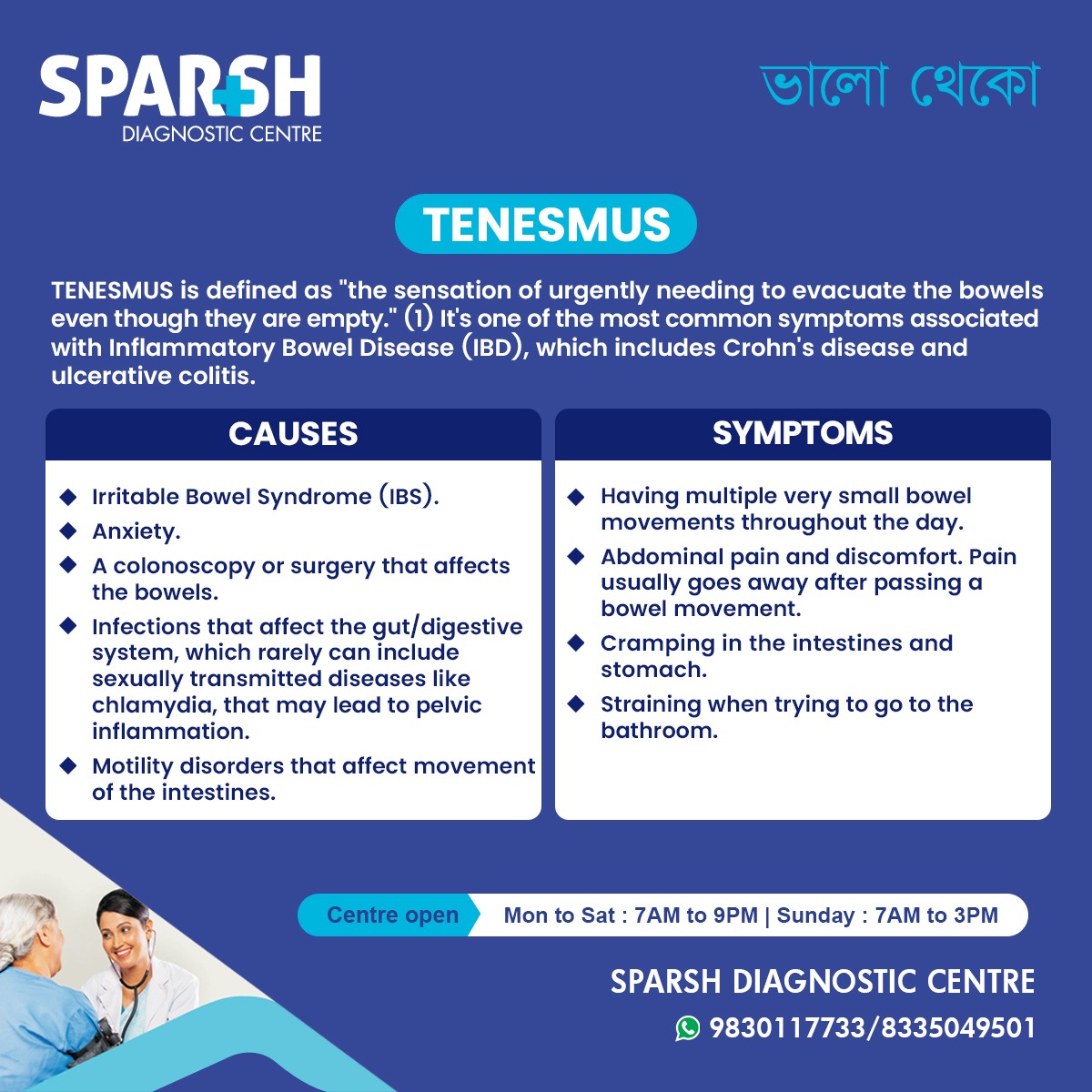
Tenesmus is a gastrointestinal symptom that can significantly affect a person’s quality of life. It is characterized by a persistent feeling of needing to empty the bowels, even after a bowel movement or when the rectum is empty. This uncomfortable and often distressing sensation is commonly associated with conditions affecting the intestines, rectum, or pelvic region.
While tenesmus itself is not a disease, it is an important warning sign that may point to underlying digestive disorders such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), infections, or rectal inflammation. Understanding tenesmus, its causes, and available treatments is essential for early diagnosis and effective management.
This article provides a comprehensive overview of tenesmus, including symptoms, causes, diagnostic methods, treatment options, and frequently asked questions.
What Is Tenesmus?
Tenesmus is defined as the sensation of urgently needing to evacuate the bowels despite little or no stool being present. The term is most commonly used to describe rectal tenesmus, which involves discomfort or pressure in the rectum.
Patients with tenesmus may feel as though their bowels are never completely empty. This sensation can occur multiple times a day and is often accompanied by pain, cramping, or straining during bowel movements.
Tenesmus is frequently seen in people with inflammatory bowel disease, including ulcerative colitis and Crohn’s disease, but it can also occur due to infections, anxiety, or structural abnormalities of the bowel.
Types of Tenesmus
1. Rectal Tenesmus
This is the most common type and involves a persistent urge to pass stool originating from the rectum. It is often linked to inflammation, infection, or tumors in the rectal area.
2. Vesical Tenesmus
Less common, this refers to a constant urge to urinate and is associated with bladder or pelvic conditions rather than the bowel.
Causes of Tenesmus
Tenesmus can result from a wide range of gastrointestinal and non-gastrointestinal conditions. Common causes include:
1. Inflammatory Bowel Disease (IBD)
Inflammation of the intestinal lining can irritate rectal nerves, causing a constant urge to defecate.
2. Irritable Bowel Syndrome (IBS)
Although IBS does not cause visible inflammation, abnormal bowel motility and heightened gut sensitivity can lead to tenesmus.
3. Gastrointestinal Infections
Bacterial, viral, or parasitic infections can inflame the intestines and rectum. In rare cases, sexually transmitted infections such as chlamydia can cause rectal inflammation leading to tenesmus.
4. Chronic Constipation
Hard or impacted stool can stretch the rectum and stimulate nerve endings, creating a false sensation of needing to pass stool.
5. Colorectal Cancer
Tumors in the rectum or colon may obstruct stool passage and irritate surrounding tissues, resulting in tenesmus.
6. Pelvic Floor Disorders
Abnormal muscle coordination during bowel movements can prevent complete evacuation and cause persistent rectal pressure.
7. Anxiety and Stress
Psychological stress can affect gut-brain communication, worsening bowel symptoms including tenesmus.
8. Post-Surgical or Post-Procedure Effects
Procedures such as colonoscopy, bowel surgery, or radiation therapy can temporarily irritate rectal tissues.
Symptoms Associated With Tenesmus
Tenesmus often occurs alongside other gastrointestinal symptoms, including:
Frequent urges to pass stool with little output
Passing very small amounts of stool multiple times a day
Rectal pain or pressure
Abdominal pain or cramping
Straining during bowel movements
Sensation of incomplete evacuation
Mucus or blood in stool (in some cases)
The severity and combination of symptoms vary depending on the underlying cause.
How Is Tenesmus Diagnosed?
Diagnosing tenesmus involves identifying the root cause rather than the symptom itself. A healthcare provider may recommend:
1. Medical History and Physical Examination
Detailed questioning about bowel habits, pain, diet, stress, and associated symptoms.
2. Stool Tests
To detect infections, inflammation, or blood in the stool.
3. Blood Tests
To check for inflammation, infection, anemia, or autoimmune markers.
4. Colonoscopy or Sigmoidoscopy
Allows direct visualization of the colon and rectum to detect inflammation, ulcers, polyps, or tumors.
5. Imaging Studies
CT scans or MRI may be used to evaluate structural abnormalities or pelvic conditions.
Early diagnosis is essential, especially when tenesmus is persistent or accompanied by alarming symptoms such as weight loss or rectal bleeding.
Treatment Options for Tenesmus
Treatment focuses on addressing the underlying cause. Management may include:
1. Medications
Anti-inflammatory drugs for IBD
Antibiotics for infections
Antispasmodics for IBS
Laxatives or stool softeners for constipation
Anxiety-reducing medications if stress is a contributing factor
2. Dietary Modifications
High-fiber diet for constipation (if appropriate)
Low-FODMAP diet for IBS
Avoiding trigger foods such as spicy or fatty meals
Adequate hydration
3. Lifestyle Changes
Regular physical activity
Stress management techniques like yoga or meditation
Establishing healthy bowel habits
4. Pelvic Floor Therapy
Helpful for patients with pelvic floor dysfunction or chronic straining.
5. Surgical Intervention
In rare cases, surgery may be required for tumors, severe IBD complications, or structural abnormalities.
When Should You See a Doctor?
Medical evaluation is recommended if tenesmus:
Persists for more than a few days
Is accompanied by blood or mucus in stool
Causes severe abdominal or rectal pain
Is associated with unexplained weight loss or fever
Interferes with daily activities or sleep
Early medical attention helps prevent complications and ensures appropriate treatment.
Can Tenesmus Be Prevented?
While not all cases can be prevented, certain measures may reduce risk:
Practicing good hygiene to prevent infections
Seeking early treatment for bowel disorders
Frequently Asked Questions (FAQs)
1. Is tenesmus a disease?
No, tenesmus is a symptom, not a disease. It usually indicates an underlying condition affecting the bowel or rectum.
2. Is tenesmus dangerous?
Tenesmus itself is not dangerous, but it may signal serious conditions such as inflammatory bowel disease or colorectal cancer, which require medical evaluation.
3. Can anxiety cause tenesmus?
Yes. Anxiety and stress can affect gut function and may trigger or worsen tenesmus, especially in people with IBS.
4. Does tenesmus always mean inflammatory bowel disease?
No. While common in IBD, tenesmus can also occur due to IBS, infections, constipation, or pelvic floor disorders.
5. How long does tenesmus last?
The duration depends on the underlying cause. It may be temporary in infections or persistent in chronic conditions like IBD.
6. Can tenesmus be cured?
Tenesmus can often be relieved or resolved by treating the underlying condition. Some chronic causes may require long-term management.
7. Should I worry if I have tenesmus without pain?
Even painless tenesmus should be evaluated if it persists, as it may indicate rectal inflammation or obstruction.
Tenesmus is a troubling and uncomfortable symptom that should not be ignored. Although it may arise from relatively benign causes such as stress or IBS, it can also be an early warning sign of more serious gastrointestinal conditions. Early diagnosis, appropriate investigations, and targeted treatment play a vital role in managing tenesmus effectively.
If you or a loved one experience persistent bowel urgency, rectal discomfort, or incomplete evacuation, consulting a healthcare professional or diagnostic centre is an important step toward relief and long-term digestive health.
To consult a Gastroenterologist at Sparsh Diagnostic Centre, call our helpline number 9830117733.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

Sparsh Diagnostic Centre Doctor List
![]()