Rabies is one of the deadliest viral diseases known to mankind. Caused by the rabies virus, it affects the central nervous system and, once symptoms appear, it is almost always fatal. The good news? Rabies is entirely preventable with timely medical intervention and proper awareness.
In this comprehensive blog, we will explore what rabies is, how it spreads, symptoms, treatment options, and preventive measures to keep yourself and your loved ones safe.
What Is Rabies?
Rabies is a viral infection caused by the rabies virus, which belongs to the Lyssavirus genus. It primarily affects warm-blooded mammals, including humans. The virus attacks the central nervous system—the brain and spinal cord—leading to inflammation, neurological damage, coma, and ultimately, death.
How Is Rabies Transmitted?
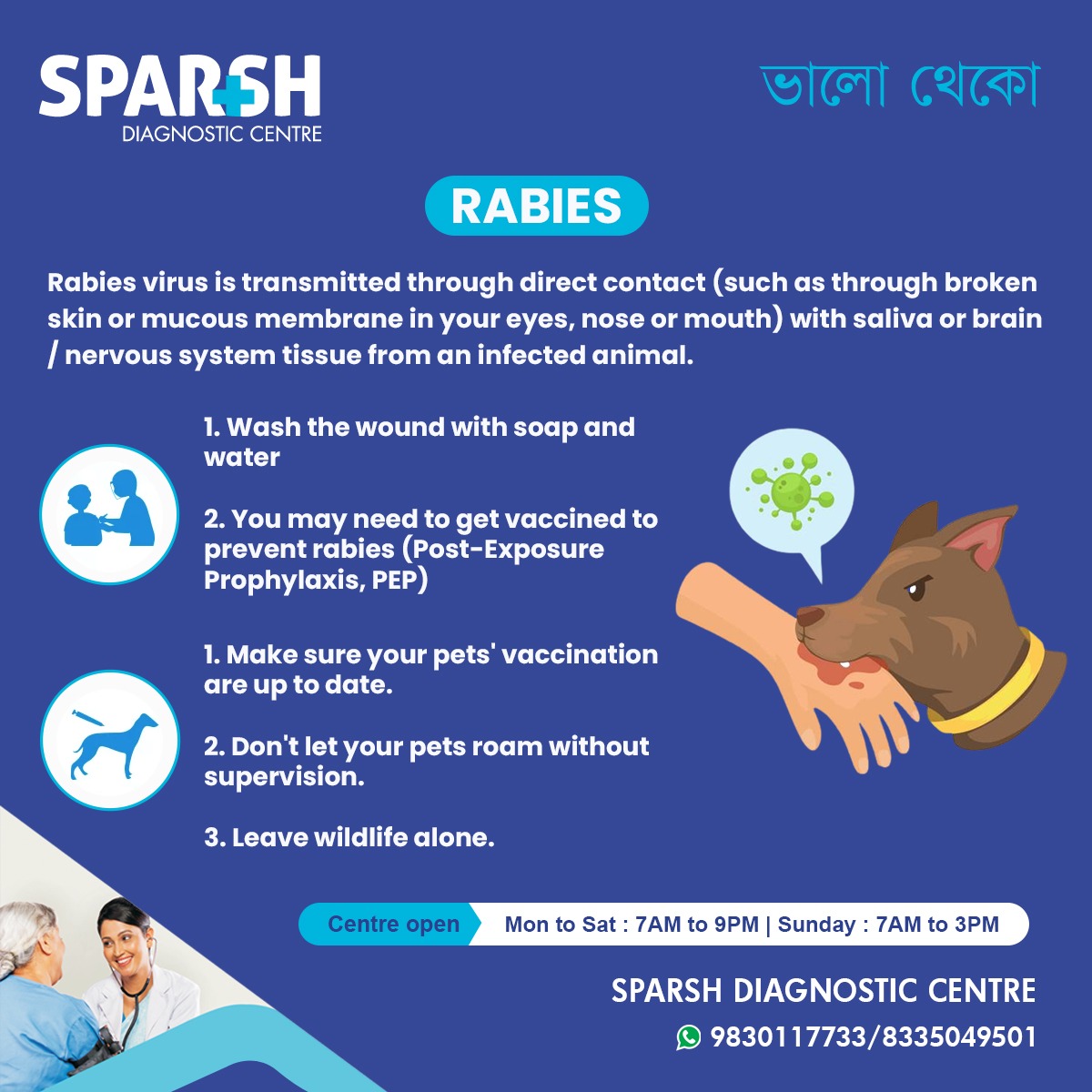
Rabies is usually transmitted through the bite or scratch of an infected animal. The virus is present in the saliva and nervous tissue of infected animals. In rare cases, it can enter the human body through mucous membranes (eyes, nose, or mouth) or open wounds that come into contact with infected saliva.
Common modes of transmission:
Dog bites (most common in India and many developing countries)
Cat scratches
Bites from wild animals like bats, raccoons, foxes, and monkeys
Exposure to brain or nervous tissue of infected animals
Animals That Commonly Spread Rabies
The majority of human rabies cases come from domestic dogs. However, the following animals can also be carriers:
Dogs
Cats
Bats
Monkeys
Raccoons
Skunks
Foxes
Coyotes
Note: Rodents like squirrels, rats, and rabbits are rarely rabies carriers.
Stages of Rabies Infection
Rabies infection occurs in stages, starting from exposure to the appearance of symptoms:
1. Incubation Period
Lasts from 1 week to 3 months (can be longer)
No symptoms
The virus slowly travels from the site of exposure to the central nervous system
2. Prodromal Stage
Lasts 2–10 days
Symptoms resemble flu:
Fever
Nausea
Pain or tingling at the bite site
Fatigue and anxiety
3. Acute Neurological Stage
Severe and alarming symptoms:
Hallucinations
Agitation
Difficulty swallowing (hydrophobia)
Excessive salivation
Muscle spasms
Seizures
Paralysis
4. Coma and Death
Once clinical symptoms appear, death usually occurs within days
Fatality rate is nearly 100%
Signs and Symptoms of Rabies
Early symptoms (within days of exposure):
Later symptoms (as the virus progresses):
Confusion
Hallucinations
Agitation
Muscle spasms
Difficulty speaking and swallowing
Hydrophobia (fear of water)
Aerophobia (fear of drafts or fresh air)
Coma
Death
Diagnosing Rabies
Rabies is difficult to diagnose before symptoms appear, which is why clinical history (animal bite or scratch) and immediate medical evaluation are crucial.
Diagnostic methods include:
Saliva testing (PCR for viral RNA)
Skin biopsy from the neck
Blood and spinal fluid antibody tests
Postmortem brain tissue examination (in animals)
What to Do After an Animal Bite or Scratch
If you or someone you know is bitten or scratched by an animal, take immediate action:
Step 1: Wound Care
Wash the wound thoroughly with soap and water for at least 15 minutes
Use an antiseptic like povidone-iodine or alcohol
Step 2: Seek Medical Attention
Go to the nearest healthcare center or diagnostic centre like Sparsh Diagnostic Centre for evaluation
Step 3: Post-Exposure Prophylaxis (PEP)
A combination of rabies vaccine and rabies immunoglobulin (RIG) is administered based on the exposure category
Rabies Exposure Categories (WHO Guidelines)
Category I:
Touching or feeding animals
Licks on intact skin
Action: No PEP needed
Category II:
Minor scratches or abrasions without bleeding
Action: Immediate vaccination
Category III:
Transdermal bites or scratches
Licks on broken skin
Exposure to saliva via mucous membranes
Action: Vaccination + Rabies Immunoglobulin (RIG)
Rabies Vaccination
1. Pre-Exposure Prophylaxis (PrEP)
Recommended for:
Veterinarians
Lab workers
Animal handlers
Travelers to high-risk areas
Schedule:
3 doses: Day 0, Day 7, Day 21 or 28
2. Post-Exposure Prophylaxis (PEP)
Unvaccinated individuals:
4 or 5 doses of vaccine (Days 0, 3, 7, 14, ±28)
Rabies Immunoglobulin (in Category III)
Previously vaccinated:
2 booster doses (Days 0 and 3)
No RIG required
Rabies in India: A Public Health Crisis
India reports the highest number of rabies deaths globally—about 20,000 annually, mostly due to dog bites. Factors include:
Lack of public awareness
Inadequate dog vaccination
Poor access to healthcare in rural areas
Organizations like WHO and NCDC India have launched initiatives to eliminate rabies by 2030.
How to Prevent Rabies
For Individuals:
Vaccinate pets regularly
Avoid contact with stray or wild animals
Supervise children around animals
Don’t allow pets to roam unsupervised
Educate yourself and your family
Avoid provoking animals
For Pet Owners:
Annual rabies vaccines for dogs and cats
Maintain updated vaccination records
Keep pets indoors or in fenced areas
Community Measures:
Control stray dog population through sterilization
Conduct mass vaccination campaigns
Spread awareness in schools and rural communities
Rabies Myths vs Facts
| Myth | Fact |
|---|---|
| Only dogs spread rabies | Many animals can transmit rabies including bats, cats, and monkeys |
| A small scratch can’t cause rabies | Even minor exposure to infected saliva can transmit the virus |
| You don’t need treatment if there’s no bleeding | Any contact with potentially infected animals requires medical attention |
| Rabies can be treated after symptoms appear | Rabies is almost always fatal after symptoms show |
| Vaccination is painful | Modern vaccines are given in the arm and are not painful like older ones |
The Role of Diagnostic Centres
Prompt diagnosis and timely vaccination are key to preventing rabies. Trusted diagnostic centres like Sparsh Diagnostic Centre provide:
Rabies vaccination (Pre and Post-Exposure)
Immunoglobulin therapy
Lab testing
Emergency wound care
Pet vaccination support
Community education programs
The “One Health” Approach to Rabies Prevention
Rabies control requires a multisectoral approach, involving:
Human health services
Animal health services
Environmental health services
Key components include:
Mass dog vaccination
Public health education
Availability of vaccines and RIG
Surveillance and response systems
Rabies is 100% preventable but 100% fatal once symptoms appear. The key to prevention lies in awareness, education, vaccination, and rapid medical response. Whether you’re a pet owner, parent, traveler, or healthcare professional, staying informed can save lives.
At Sparsh Diagnostic Centre, we are committed to fighting rabies through awareness, vaccination services, and rapid post-exposure care. If you or someone you know has been bitten or scratched by an animal, don’t wait—visit us immediately.
Frequently Asked Questions (FAQs)
1. Can you survive rabies once symptoms appear?
Survival is extremely rare. Rabies is almost always fatal after symptoms develop.
2. How soon after a bite should I get the rabies vaccine?
Immediately. The sooner the vaccine is administered, the more effective it is.
3. Is rabies curable?
No, there is no cure once clinical symptoms appear. Preventive vaccination is the only protection.
4. Can cats and monkeys transmit rabies?
Yes, all warm-blooded mammals, including cats and monkeys, can carry and transmit the virus.
5. Is there a test to confirm rabies in humans?
Yes, but it’s difficult and often not helpful once symptoms begin. Clinical diagnosis is prioritized based on history and symptoms.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()






[…] Examples: Inactivated Polio Vaccine (IPV), Hepatitis A, Rabies […]
[…] Rabies virus […]
[…] Viral Infections: The most common cause, including herpes simplex virus (HSV), West Nile virus, and rabies. […]