Protein-energy malnutrition (PEM) is one of the most serious nutritional problems affecting children in many developing regions of the world. Among the different forms of PEM, Kwashiorkor and Marasmus are the two major types. Though both are caused by nutritional deficiencies, they differ greatly in their clinical presentation, causes, and long-term outcomes.
Understanding the differences is crucial for early diagnosis, appropriate treatment, and prevention. In this comprehensive guide, we break down Kwashiorkor vs Marasmus, symptoms, causes, complications, diagnosis, treatment options, and prevention tips.
What Are Kwashiorkor and Marasmus?
Kwashiorkor and marasmus are both forms of severe acute malnutrition (SAM).
Kwashiorkor
Primarily caused by severe protein deficiency.
Calories may be adequate, especially from carbohydrates, but protein intake is extremely low.
The condition is marked by edema (swelling), fatty liver, and changes in skin and hair.
Marasmus
Caused by deficiency of both calories and protein.
The child appears extremely emaciated due to loss of subcutaneous fat and muscle.
There is no edema; weight loss is dramatic.
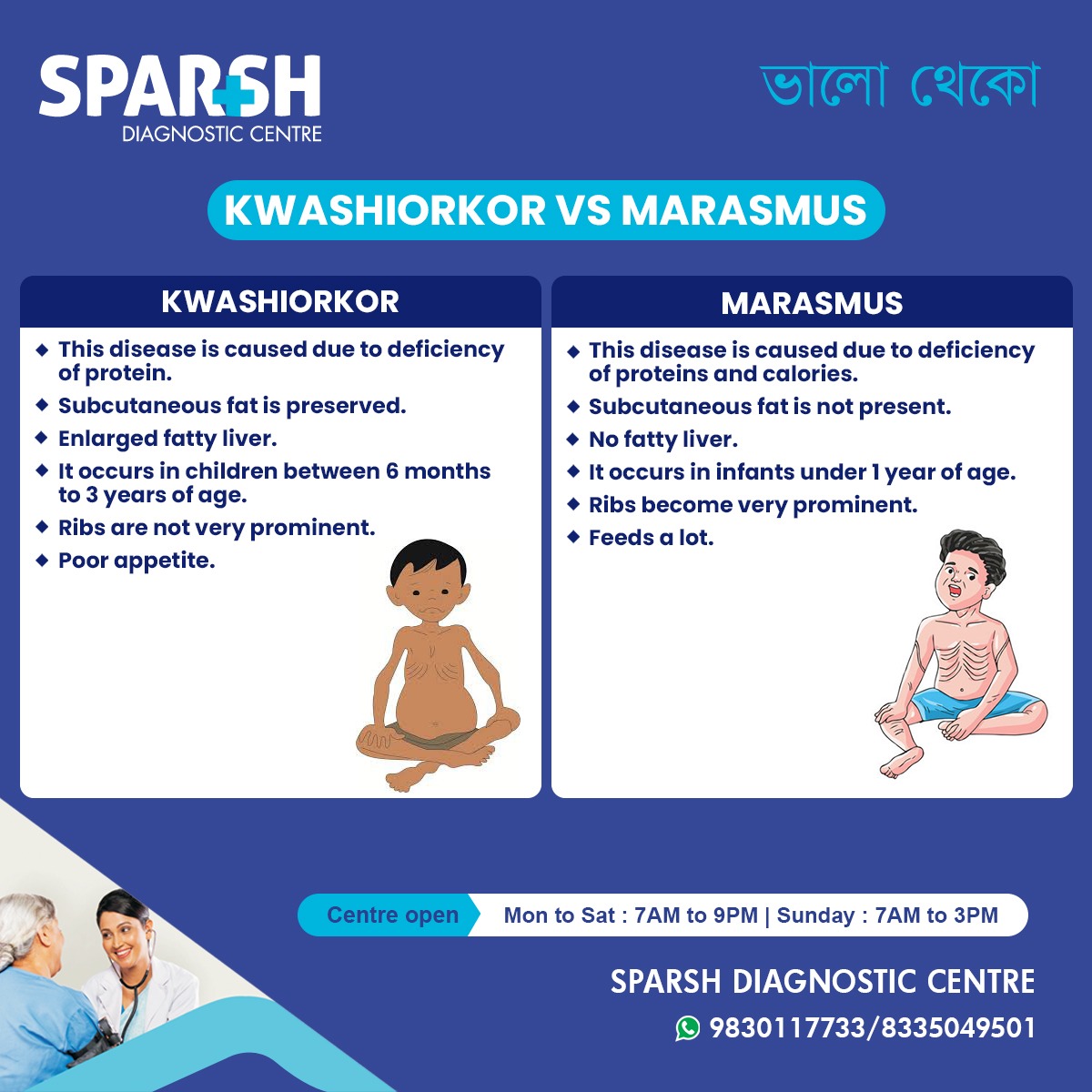
Kwashiorkor vs Marasmus: Quick Comparison Table
| Feature | Kwashiorkor | Marasmus |
|---|---|---|
| Main Cause | Severe protein deficiency | Deficiency of both calories and proteins |
| Age Group | 6 months to 3 years | Usually < 1 year |
| Subcutaneous Fat | Preserved | Lost; fat not present |
| Liver | Fatty liver enlarged | No fatty liver |
| Ribs Visibility | Not very prominent | Ribs very prominent |
| Appetite | Poor | Usually good; eats more |
| Edema | Present (swelling) | Absent |
| Appearance | Moon-face, swollen legs, flaky skin | Extremely thin, wrinkled skin, old-man appearance |
| Hair Changes | Sparse, reddish, easily plucked | Rare hair changes |
| Mortality Risk | Higher if untreated | High but slightly lower than kwashiorkor |
Understanding Kwashiorkor in Detail
Kwashiorkor is caused primarily by a lack of dietary protein, even when there is sufficient energy intake. This often happens in communities where the diet is high in carbohydrates (rice, cassava, sweet potatoes) but low in proteins (milk, eggs, meat, legumes).
Key Symptoms
Enlarged and fatty liver
Subcutaneous fat preserved
Stunted growth
Flaky paint dermatitis
Irritability and apathy
Changes in hair texture and color
Poor appetite
Why Does Edema Occur?
Lack of protein leads to reduced albumin levels in the blood. Albumin helps maintain osmotic pressure; without it, fluid leaks from blood vessels into tissues, causing swelling.
Risk Factors
Early weaning
Diet high in starch but low in protein
Poverty and famine
Repeated infections
Lack of awareness about balanced diet
Understanding Marasmus in Detail
Marasmus results from overall energy deficiency, meaning the child is not getting enough calories or protein. It is most common in infants who are not adequately breastfed or are treated with diluted formula.
Key Symptoms
Extreme wasting and thinness
Loss of subcutaneous fat
Prominent bones & ribs
Old-man appearance
Wrinkled skin
Good or increased appetite
No edema
Irritable but alert
Very low weight-for-age
Why Is Appetite Good in Marasmus?
As the child experiences starvation, hunger hormones increase, leading to a strong desire to eat — unlike kwashiorkor, where appetite is suppressed.
Risk Factors
Severe poverty
Chronic starvation
Diluted infant formula
Early cessation of breastfeeding
Infections causing poor nutrient absorption
Major Differences Between Kwashiorkor and Marasmus
1. Type of Nutrient Deficiency
Kwashiorkor = protein deficiency
Marasmus = protein + calorie deficiency
This is the fundamental difference.
2. Body Appearance
Kwashiorkor: swollen body due to edema; preserved fat
Marasmus: extremely thin, no fat or muscle
3. Liver Condition
Kwashiorkor: fatty liver (hepatic steatosis)
Marasmus: normal liver
4. Age Group
Kwashiorkor: typically 6 months to 3 years
Marasmus: under 1 year, especially infants
5. Appetite
Kwashiorkor: poor appetite
Marasmus: good appetite
6. Hair and Skin Changes
Kwashiorkor: flaky skin, hair depigmentation
Marasmus: skin dry but no major hair changes
Causes of Kwashiorkor and Marasmus
Common Causes
Both conditions may occur due to:
Poverty
Famine or natural disasters
Poor feeding practices
Limited access to nutrient-rich foods
Chronic illnesses
Malabsorption disorders
Condition-Specific Causes
Kwashiorkor
Low-protein diet
High carbohydrate intake
Liver unable to synthesize protein
Frequent infections
Marasmus
Severe calorie restriction
Inadequate breastfeeding
Malabsorption disorders (celiac disease, cystic fibrosis)
Diagnosis of Kwashiorkor and Marasmus
Healthcare professionals use:
Physical examination
Weight-for-height or weight-for-age measurements
MUAC (mid-upper arm circumference)
Blood tests (albumin, total protein)
Electrolyte profile
Edema is a key diagnostic marker distinguishing Kwashiorkor from Marasmus.
Treatment and Management
Both conditions require urgent medical care. The treatment protocol usually follows WHO guidelines.
1. Stabilization Phase (First 1–2 days)
Treat dehydration
Correct electrolyte imbalance
Give antibiotics
Manage hypoglycemia and hypothermia
Start low-protein, low-lactose therapeutic feeding (F-75 formula)
2. Transition Phase
Gradually increase caloric intake
Treat vitamin and mineral deficiencies
Manage infections and diarrhea
3. Rehabilitation Phase
Introduce F-100 formula
Add protein-rich foods
Nutritional counseling for parents
Monitor growth regularly
Complications if Untreated
Severe infections
Growth failure or short stature
Cognitive impairment
Death (Kwashiorkor has a higher mortality rate)
Prevention of Kwashiorkor and Marasmus
1. Promote exclusive breastfeeding for 6 months
Breast milk contains essential proteins, calories, and antibodies.
2. Introduce protein-rich complementary foods
After 6 months:
Eggs
Fish
Lentils, beans
Milk and yogurt
3. Regular health check-ups
Helps detect early signs of malnutrition.
4. Improve maternal nutrition
Healthy mothers produce nutrient-rich breast milk.
5. Community education
Awareness about balanced diet prevents misinformed feeding practices.
Kwashiorkor and Marasmus are severe forms of malnutrition, but they differ widely in causes, symptoms, and physical appearance. Kwashiorkor results mainly from protein deficiency, whereas marasmus is caused by both calorie and protein deficiency. Early recognition and rapid treatment can save a child’s life and ensure healthy development.
Sparsh Diagnostic Centre emphasises early diagnosis, awareness, and preventive care to reduce the burden of malnutrition in children. If you suspect malnutrition in a child, timely medical evaluation is essential.
FAQ Section
1. What is the major difference between Kwashiorkor and Marasmus?
Kwashiorkor is caused by protein deficiency, while marasmus is caused by overall calorie and protein deficiency.
2. Why is there swelling in Kwashiorkor?
Swelling (edema) occurs due to low albumin levels, which cause fluid to leak into tissues.
3. Can a child have both Kwashiorkor and Marasmus?
Yes. In such cases, it’s called Marasmic-Kwashiorkor, a mixed form of malnutrition.
4. Which condition is more dangerous?
Both are serious, but Kwashiorkor often has a higher mortality rate due to complications like infections and liver dysfunction.
5. Can malnutrition affect brain development?
Yes. Severe malnutrition can impair cognitive development, learning ability, and overall growth.
6. How is severe malnutrition diagnosed?
Doctors use physical examination, weight-for-height measurements, MUAC, blood tests, and liver function tests.
7. Can Kwashiorkor and Marasmus be fully cured?
With early diagnosis and proper treatment, most children can recover fully, although long-term effects may persist if treatment is delayed.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()