Your veins play a crucial role in returning blood from your legs back to the heart. To achieve this, they rely on one-way valves that prevent blood from flowing backward. However, when these valves weaken or become damaged, blood can pool in the legs, leading to a condition called Chronic Venous Insufficiency (CVI).
CVI is a long-term health issue that affects millions worldwide, especially adults over 50 and individuals with a history of varicose veins or deep vein thrombosis (DVT). Left untreated, it can cause significant discomfort, skin changes, and even painful ulcers.
This article explores everything you need to know about Chronic Venous Insufficiency—from causes and risk factors to symptoms, diagnosis, treatment, and prevention.
What is Chronic Venous Insufficiency?
Chronic Venous Insufficiency (CVI) is a medical condition where the veins in the legs cannot efficiently pump blood back to the heart. Instead, blood collects (pools) in the veins, leading to increased pressure, swelling, and damage to the vein walls and skin.
Unlike temporary swelling caused by long flights or standing for extended periods, CVI is a progressive condition that worsens over time without proper care.
Causes of Chronic Venous Insufficiency
CVI primarily results from damaged or weakened vein valves. These valves normally keep blood moving upward against gravity. When they fail, blood flows backward (venous reflux), creating congestion.
Common causes include:
Deep Vein Thrombosis (DVT): A blood clot in the deep veins can damage valves permanently.
Varicose Veins: Enlarged, twisted veins caused by faulty valves increase the risk of CVI.
Obesity: Extra body weight increases pressure on leg veins.
Pregnancy: Hormonal changes and increased blood volume can strain veins.
Prolonged Standing or Sitting: Occupations like teaching, nursing, and office work contribute to poor blood circulation.
Genetics: Family history of vein problems increases susceptibility.
Age and Gender: Older adults and women are more prone due to hormonal influences.
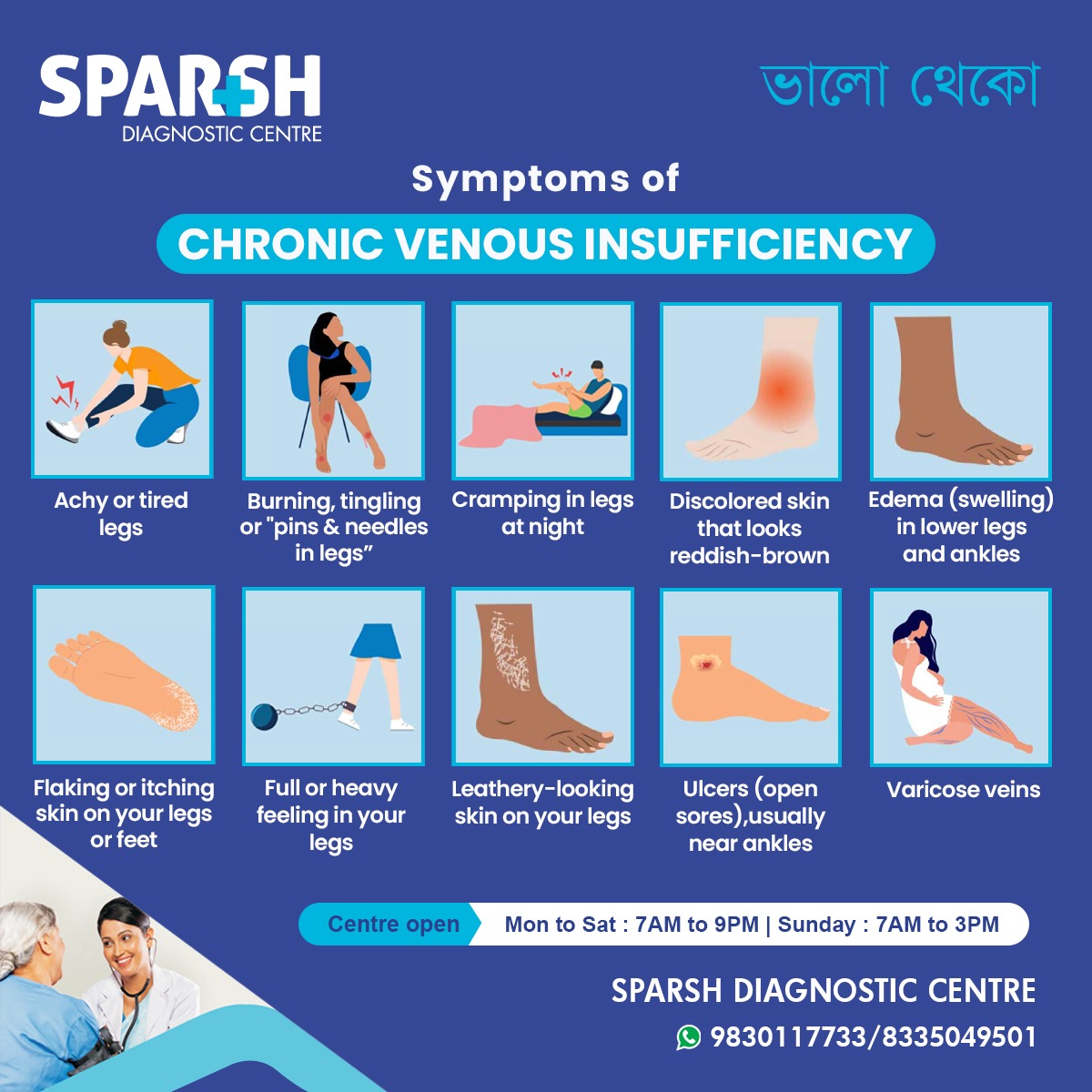
Symptoms of Chronic Venous Insufficiency
The symptoms of CVI develop gradually and worsen over time. Many people dismiss early signs as simple fatigue, but recognizing them early is crucial for effective treatment.
Key symptoms include:
Achy or tired legs – Persistent leg fatigue, especially after standing or walking.
Burning, tingling, or “pins & needles” sensation in legs – Caused by poor circulation.
Cramping in your legs at night – A common sign of venous reflux.
Discolored skin that looks reddish-brown – Especially around ankles and calves.
Edema (swelling) in lower legs and ankles – Fluid buildup due to poor blood flow.
Flaking or itching skin on your legs or feet – Indicating venous eczema.
Full or heavy feeling in your legs – A hallmark sign of blood pooling.
Leathery-looking skin on your legs – A result of long-term skin damage.
Ulcers (open sores), usually near ankles – Severe cases may develop painful wounds.
Varicose veins – Twisted, bulging veins visible under the skin.
Stages of Chronic Venous Insufficiency
Doctors often classify CVI using the CEAP system (Clinical, Etiological, Anatomical, Pathophysiological):
C0: No visible signs, but symptoms like heaviness exist.
C1: Small veins or spider veins visible.
C2: Varicose veins present.
C3: Swelling (edema) occurs.
C4: Skin changes like discoloration or eczema.
C5: Healed venous ulcers.
C6: Active venous ulcers.
This staging helps guide treatment options.
Complications of Chronic Venous Insufficiency
If left untreated, CVI can cause:
Chronic pain and swelling
Non-healing ulcers near the ankles
Blood clots (superficial thrombophlebitis or DVT)
Reduced mobility and quality of life
Diagnosis of Chronic Venous Insufficiency
If you notice symptoms of CVI, consult a healthcare provider. Diagnosis typically involves:
Medical history and physical exam – Checking visible veins, swelling, or skin changes.
Duplex ultrasound – A non-invasive test that shows blood flow and detects valve problems.
Venography (rarely used) – X-ray imaging with contrast dye to visualize veins.
Treatment Options for Chronic Venous Insufficiency
Treatment depends on the severity of the condition. The primary goals are to improve blood flow, reduce symptoms, and prevent complications.
1. Lifestyle Modifications
Exercise regularly (walking, cycling, swimming) to improve circulation.
Elevate legs above heart level for 15–30 minutes daily.
Avoid prolonged sitting or standing to reduce vein pressure.
Maintain a healthy weight to reduce stress on veins.
Wear comfortable shoes and avoid high heels.
2. Compression Therapy
Compression stockings improve blood flow by gently squeezing the legs.
Available in different pressure levels, they are often the first line of treatment.
3. Medications
Diuretics (for swelling in some cases).
Venoactive drugs (like horse chestnut extract, micronized purified flavonoid fraction).
Pain relievers for discomfort.
Anticoagulants (blood thinners) if DVT risk exists.
4. Minimally Invasive Procedures
Sclerotherapy: Injection of a solution to close off damaged veins.
Endovenous Laser Therapy (EVLT): Uses laser energy to seal faulty veins.
Radiofrequency Ablation (RFA): Heat-based treatment to close veins.
5. Surgical Treatments
Vein ligation and stripping: Removal of large varicose veins.
Ambulatory phlebectomy: Small incisions to remove surface veins.
Bypass surgery: Rare, reserved for severe cases.
Prevention of Chronic Venous Insufficiency
While not all cases can be prevented, you can lower your risk by:
Staying physically active.
Maintaining a healthy body weight.
Taking breaks during long periods of sitting or standing.
Wearing compression stockings if you have a family history.
Living with Chronic Venous Insufficiency
CVI is a lifelong condition but can be managed effectively. Regular follow-ups, a healthy lifestyle, and early treatment of symptoms can significantly improve quality of life. With proper care, severe complications like ulcers and infections can be avoided.
Frequently Asked Questions (FAQ) About Chronic Venous Insufficiency
Q1: Is Chronic Venous Insufficiency the same as varicose veins?
No. Varicose veins are a symptom of CVI, but not all varicose veins lead to CVI. CVI is a more advanced condition involving poor vein function.
Q2: Can Chronic Venous Insufficiency be cured?
CVI cannot be completely cured, but symptoms can be managed, and progression can be slowed with lifestyle changes, compression therapy, and treatments.
Q3: Who is most at risk of CVI?
People over 50, women, obese individuals, pregnant women, and those with a history of DVT or varicose veins are at higher risk.
Q4: When should I see a doctor?
If you notice persistent leg swelling, skin changes, ulcers, or painful varicose veins, consult a doctor immediately.
Q5: Do compression stockings really help?
Yes. They are one of the most effective non-surgical treatments for improving blood flow and reducing symptoms.
Q6: Can exercise help CVI?
Yes. Walking, cycling, and swimming strengthen calf muscles, which act as a “pump” to push blood upward.
Q7: Are ulcers from CVI dangerous?
Yes. They can get infected and become very difficult to heal. Immediate medical attention is necessary.
Chronic Venous Insufficiency (CVI) is a progressive condition that affects the veins in your legs, leading to discomfort, swelling, skin changes, and ulcers if untreated. Early recognition of symptoms like achy legs, swelling, discoloration, varicose veins, and skin changes can prevent severe complications.
With lifestyle changes, compression therapy, medications, and minimally invasive treatments, CVI can be effectively managed, helping patients live healthier and more active lives.
If you experience any symptoms of CVI, don’t ignore them—consult a doctor at Sparsh Diagnostic Centre for diagnosis and treatment.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()