Understanding the early signs and risk factors of peritonitis can help in early diagnosis and timely treatment. This comprehensive guide covers everything you need to know about peritonitis—its symptoms, types, causes, diagnosis, treatment options, complications, and prevention.
What is Peritonitis?
Peritonitis refers to inflammation of the peritoneum, the protective lining of the abdomen. It can affect part of the abdomen or spread throughout the entire abdominal cavity. The condition can develop suddenly (acute peritonitis) or gradually (chronic peritonitis).
Peritonitis is considered a medical emergency because the infection can quickly enter the bloodstream and result in septic shock, a life-threatening condition.
Types of Peritonitis
There are three major types:
1. Primary Peritonitis (Spontaneous Bacterial Peritonitis – SBP)
This form typically occurs in people with:
It is usually caused by bacteria entering the peritoneal cavity from the bloodstream or lymphatic system rather than from a perforation.
2. Secondary Peritonitis
This is the most common type and occurs when an infection or leakage originates within the abdominal organs.
Common causes include:
Ruptured appendix
Perforated peptic ulcer
Trauma or injury
Bowel obstruction
Leakage after abdominal surgery
3. Tertiary Peritonitis
A persistent or recurrent infection that may occur even after appropriate treatment. It is usually seen in:
Immunocompromised patients
Patients in intensive care
Those with severe underlying illnesses
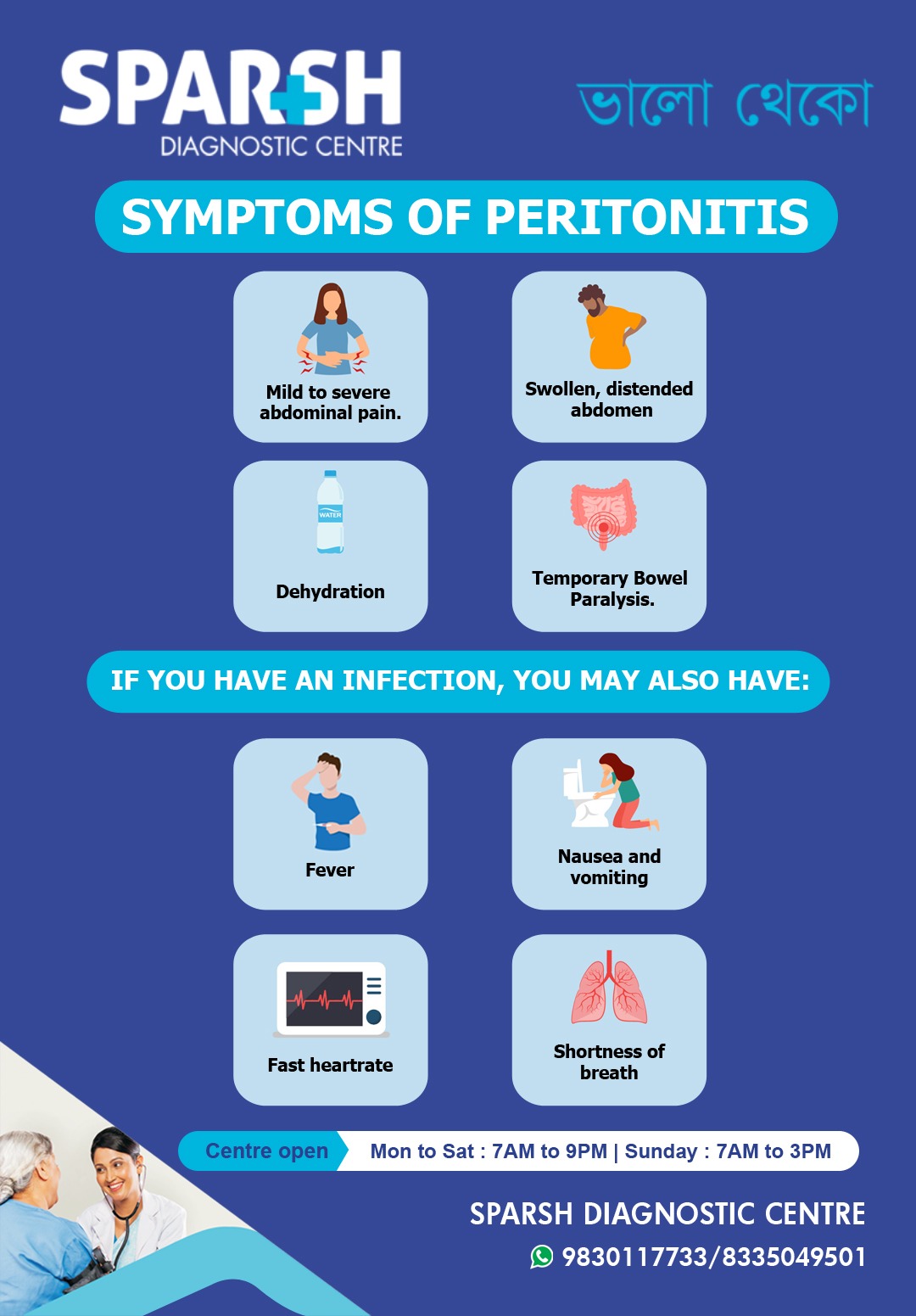
Symptoms of Peritonitis
The symptoms may differ based on the underlying cause but commonly include:
1. Mild to Severe Abdominal Pain
Abdominal pain is usually intense, sharp, and worsens with movement or touch. Patients often avoid movement to reduce discomfort.
2. Swollen and Distended Abdomen
The abdomen may appear enlarged due to the buildup of pus, air, infection, or fluid.
3. Dehydration
Symptoms like dry mouth, low urine output, and extreme thirst may occur due to vomiting or infection.
4. Temporary Bowel Paralysis (Ileus)
The intestines may stop functioning, leading to:
Inability to pass gas
If you have an infection, you may also experience:
Untreated peritonitis can quickly lead to systemic infection and sepsis.
Causes of Peritonitis
The condition occurs when bacteria, fungi, or chemical irritants enter the peritoneal space.
Common Causes Include:
1. Perforation of Abdominal Organs
A hole or rupture in the stomach, intestines, or colon can allow digestive juices and bacteria to leak into the abdomen.
Examples:
Peptic ulcer perforation
Ruptured appendix
Traumatic bowel perforation
2. Infections
Tuberculosis in rare cases (TB peritonitis)
Spontaneous bacterial infection in people with cirrhosis
3. Medical Procedures
Dialysis catheter infections (particularly in peritoneal dialysis patients)
Post-surgical complications
Endoscopic procedures
4. Injury or Trauma
Accidents, stab wounds, and blunt force trauma can tear abdominal organs or introduce bacteria.
Diagnosis of Peritonitis
Early diagnosis is crucial for preventing complications. Doctors use a combination of physical examination, imaging tests, and laboratory tests.
1. Physical Examination
Severe tenderness
Guarding (abdominal muscles stiffen)
Rebound tenderness
Abdominal distension
2. Blood Tests
Elevated white blood cell count
Elevated CRP
Signs of sepsis
3. Imaging Tests
Ultrasound: Detects fluid accumulation
CT Scan: Identifies perforations, abscesses, obstructions
X-ray: Shows air under the diaphragm indicating perforation
4. Paracentesis
A sample of abdominal fluid is drawn to check for:
Bacteria
White blood cells
Protein levels
Treatment of Peritonitis
Treatment must begin immediately. The approach depends on the cause and severity.
1. Antibiotic Therapy
Broad-spectrum antibiotics are started immediately to control infection. Once the specific bacteria are identified, targeted antibiotics are used.
2. Surgery
Emergency surgery may be required for:
Perforated ulcers
Ruptured intestines
Peritonitis due to trauma
Abscess drainage
3. Fluid Replacement
IV fluids help stabilize blood pressure and prevent dehydration.
4. Pain Management
Analgesics may be administered, but only after diagnosis to avoid masking symptoms.
5. Peritoneal Dialysis Catheter Removal
If the infection is caused by a contaminated catheter, it may need removal.
Possible Complications of Peritonitis
If not treated quickly, peritonitis can lead to:
Septic shock
Scar tissue formation in the abdomen
Chronic digestive issues
Death
The risk increases significantly when treatment is delayed.
Prevention of Peritonitis
While not all cases can be prevented, certain steps can reduce the risk:
1. Manage Chronic Diseases
Treat cirrhosis early
Manage kidney disease
Control diabetes
2. Avoid Peritoneal Dialysis Contamination
Maintain hygiene
Follow proper catheter care techniques
Wear sterile gloves
3. Prompt Treatment of Abdominal Pain
Never ignore severe or sudden abdominal pain—it can be a sign of perforation or infection.
4. Safe Surgical Practices
Ensuring sterile techniques during surgeries reduces postoperative infection risks.
Diet and Lifestyle Tips for Recovery
After treatment for peritonitis, patients should:
Drink plenty of fluids
Follow a soft or liquid diet initially
Avoid spicy and fatty foods
Include probiotics after consulting a doctor
Avoid alcohol, especially in liver disease
immediate medical help if you experience:
Severe abdominal pain
Persistent vomiting
Fever with abdominal swelling
Difficulty breathing
Rapid heartbeat
Signs of shock (cold skin, confusion, fainting)
FAQs on Peritonitis
1. Is peritonitis life-threatening?
Yes. Peritonitis is a medical emergency that requires prompt treatment to prevent sepsis and organ failure.
2. Can peritonitis heal on its own?
No. It always requires medical treatment such as antibiotics or surgery.
3. What is spontaneous bacterial peritonitis (SBP)?
SBP occurs without an obvious cause and is common in people with liver cirrhosis and ascites.
4. What does peritonitis pain feel like?
It is usually severe, sharp, and worsens with movement or touch.
5. How is peritonitis confirmed?
Doctors use clinical examination, imaging (CT scan or ultrasound), and abdominal fluid tests.
6. Can peritonitis return?
Yes, especially in people with chronic liver disease or those undergoing peritoneal dialysis.
7. What foods should be avoided during recovery?
Avoid spicy foods, alcohol, oily dishes, and high-fat meals.
8. Is peritonitis contagious?
No, but the underlying infections causing it may spread.
Peritonitis is a severe condition that demands early detection and urgent treatment. Recognizing symptoms like severe abdominal pain, swelling, fever, or dehydration can help in seeking timely medical help. With prompt diagnosis, antibiotics, surgery when needed, and proper supportive care, patients can recover fully. Maintaining good hygiene, managing chronic diseases, and following medical guidance can significantly reduce the risk of developing peritonitis.
If you or a loved one experiences sudden abdominal symptoms, consult a healthcare professional immediately.
To consult a Doctor for treatment of peritonitis, call Sparsh Diagnostic Centre on 9830117733.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

![]()






[…] Peritonitis […]
[…] into the abdomen or chest, causing peritonitis or […]
[…] Abdominal infections: Such as peritonitis. […]
[…] When the appendix is blocked, bacteria can multiply rapidly, causing the appendix to become inflamed and swollen. If not treated promptly, the appendix can rupture, spreading infection throughout the abdomen and leading to a potentially life-threatening condition known as peritonitis. […]