Maintaining the right balance of minerals in the body is essential for good health. Among these, phosphorus plays a key role in building strong bones, producing energy, and supporting muscle and nerve functions. However, when phosphorus levels become excessively high in the bloodstream—a condition known as Hyperphosphatemia—it can lead to serious health complications, especially for individuals with kidney disease.
This comprehensive guide explains everything you need to know about Hyperphosphatemia, including its causes, symptoms, diagnostic methods, treatment options, preventive measures, and commonly asked questions.
What is Hyperphosphatemia?
Hyperphosphatemia refers to abnormally high levels of phosphate in the blood. Phosphate is a vital mineral found in bones, teeth, and cells. Normally, the kidneys regulate phosphate levels by filtering excess phosphate out of the body through urine. When the kidneys cannot efficiently remove phosphate, or when there is excessive phosphate intake or cellular breakdown, phosphate levels rise.
A normal serum phosphate level in adults is generally around 2.5–4.5 mg/dL. Levels above this range indicate Hyperphosphatemia.
This condition is most commonly associated with chronic kidney disease (CKD) but can occur due to other metabolic or dietary factors.
Causes of Hyperphosphatemia
Several underlying conditions and external factors can lead to elevated phosphate levels. The major causes include:
1. Chronic Kidney Disease (CKD)
The kidneys are primarily responsible for filtering phosphate. When kidney function declines, phosphate accumulates in the bloodstream. This makes CKD the leading cause of hyperphosphatemia.
2. Excessive Phosphate Intake
Phosphate enters the body through:
High-phosphate foods
Phosphate-containing laxatives or enemas
Processed meats and carbonated beverages with phosphoric acid
Consuming high amounts of phosphate, especially through supplements, can lead to elevated levels.
3. Hypoparathyroidism
The parathyroid hormone (PTH) regulates calcium and phosphate balance. Low PTH levels result in decreased phosphate excretion, causing accumulation.
4. Tumor Lysis Syndrome
Cancer therapies may cause rapid breakdown of tumor cells, releasing phosphate suddenly into the blood.
5. Rhabdomyolysis
Muscle injury triggers the release of large amounts of intracellular phosphate.
6. Diabetic Ketoacidosis (DKA)
Insulin deficiency and metabolic imbalance can interfere with phosphate handling.
7. Liver Disease
Liver dysfunction can affect phosphate metabolism, contributing to elevated blood levels.
8. Excess Vitamin D
Vitamin D enhances phosphate absorption from the gut. Over-supplementation may cause phosphate overload.
Symptoms of Hyperphosphatemia
In many individuals, hyperphosphatemia may be asymptomatic. Symptoms usually appear when the condition becomes severe or when calcium levels drop as a result of phosphate imbalance.
Common symptoms include:
1. Muscle Cramps or Spasms
High phosphate levels can lower calcium, leading to muscle-related issues.
2. Joint Pain
Calcium-phosphate crystals may deposit in joints, causing stiffness and discomfort.
3. Tingling or Numbness
Low calcium can cause tingling sensations, especially around the mouth and extremities.
4. Skin Itching (Pruritus)
Persistent itching is common, particularly among CKD patients.
5. Weak Bones
Chronic elevation of phosphate stimulates the parathyroid glands, eventually leading to bone demineralization.
6. Soft Tissue Calcification
Severe hyperphosphatemia may lead to calcium-phosphate deposits in:
Skin
Lungs
Blood vessels
Heart valves
This condition increases the risk of cardiovascular complications.
7. Symptoms in CKD Patients
Patients may also experience:
Bone pain
due to chronic mineral imbalance.
Complications of Hyperphosphatemia
If not managed properly, hyperphosphatemia can lead to dangerous complications such as:
1. Vascular Calcification
Calcium and phosphate deposits can harden and narrow the arteries, increasing the risk of heart attack and stroke.
2. Bone Disorders
Prolonged imbalance leads to renal osteodystrophy, weakening bones and increasing fracture risk.
3. Heart Problems
Calcifications in the heart valves may impair heart function.
4. Kidney Stone Formation
High phosphate levels contribute to stone development.
5. Chronic Mineral and Bone Disorder (CKD-MBD)
A major issue in CKD that affects the bones, heart, and overall metabolism.
Diagnosis of Hyperphosphatemia
Doctors use several tests to diagnose the condition and determine its root cause.
1. Blood Tests
These measure:
Serum phosphate
Calcium
Parathyroid hormone
Vitamin D
2. Urine Tests
Help assess how much phosphate the kidneys excrete.
3. Imaging Tests
Used to detect calcification or bone disease:
4. Medical & Dietary Review
Doctors review your diet, medications, and supplements to identify phosphate sources.
Treatment Options for Hyperphosphatemia
Treating hyperphosphatemia focuses on correcting phosphate levels and addressing underlying causes.
1. Diet Modification
Reducing phosphate intake is essential. Foods high in phosphate include:
Meat and fish
Dairy products
Nuts and seeds
Processed food
Cola drinks
Chocolate
2. Phosphate Binders
These medications block phosphate absorption from food. Types include:
Calcium-based
Non-calcium binders (sevelamer, lanthanum)
Magnesium-based binders
Commonly used for CKD patients.
3. Dialysis
Helps remove excess phosphate in advanced kidney disease.
4. Vitamin D Adjustments
Doctors may adjust vitamin D doses to prevent excess absorption.
5. Treating Underlying Conditions
Managing issues such as parathyroid disorders, liver disease, DKA, or muscle injury helps stabilize phosphate levels.
6. Adequate Hydration
Water supports kidney filtration and phosphate excretion.
Diet Tips for Managing Hyperphosphatemia
Foods to Avoid or Limit
Cheese, paneer, milk
Red meat, organ meat
Nuts, seeds
Dark cola beverages
Processed or instant food
Bran cereals
Foods to Prefer
Fresh vegetables
Fruits
Rice
Egg whites
Clear sodas
White bread
Cooking Suggestions
Boiling reduces phosphate content.
Avoid packaged foods with labels including “phosphate” or “phosphoric acid.”
Prevention of Hyperphosphatemia
1. Regular Kidney Function Monitoring
Early diagnosis of kidney issues helps prevent phosphate buildup.
2. Monitor Dietary Intake
Avoid excessive phosphate from food and supplements.
3. Hydration
Supports kidney health and mineral excretion.
4. Follow Medical Advice on Supplements
Only take vitamin D or calcium supplements when prescribed.
5. Manage Chronic Illnesses
Good control of diabetes, thyroid issues, and liver disorders helps regulate mineral balance.
When to Seek Medical Help
Consult a doctor if you notice:
Persistent muscle cramps
Tingling sensations
Bone pain
Severe itching
Signs of kidney trouble
Prompt treatment prevents serious complications.
Frequently Asked Questions (FAQ)
1. What causes hyperphosphatemia?
The most common cause is chronic kidney disease, where the kidneys cannot filter phosphate properly.
2. Can diet alone lead to high phosphate levels?
Yes, excessive intake of phosphate-rich foods or supplements can raise levels.
3. What foods should I avoid?
Avoid dairy, red meat, nuts, chocolate, processed foods, and cola drinks.
4. Is hyperphosphatemia dangerous?
If untreated, it can cause vascular calcification, bone disease, and heart issues.
5. What are normal phosphate levels?
Typically 2.5–4.5 mg/dL.
6. Can it be cured?
It can be managed effectively, especially when underlying conditions are treated.
7. How is it diagnosed?
Through blood tests, kidney function tests, urine tests, and imaging.
8. Are phosphate binders safe?
Yes, under medical supervision.
9. Does drinking water help?
Hydration supports kidney function but cannot treat severe cases alone.
10. Are symptoms always present?
No, many people do not show symptoms initially.
#BhaloTheko
Disclaimer:
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
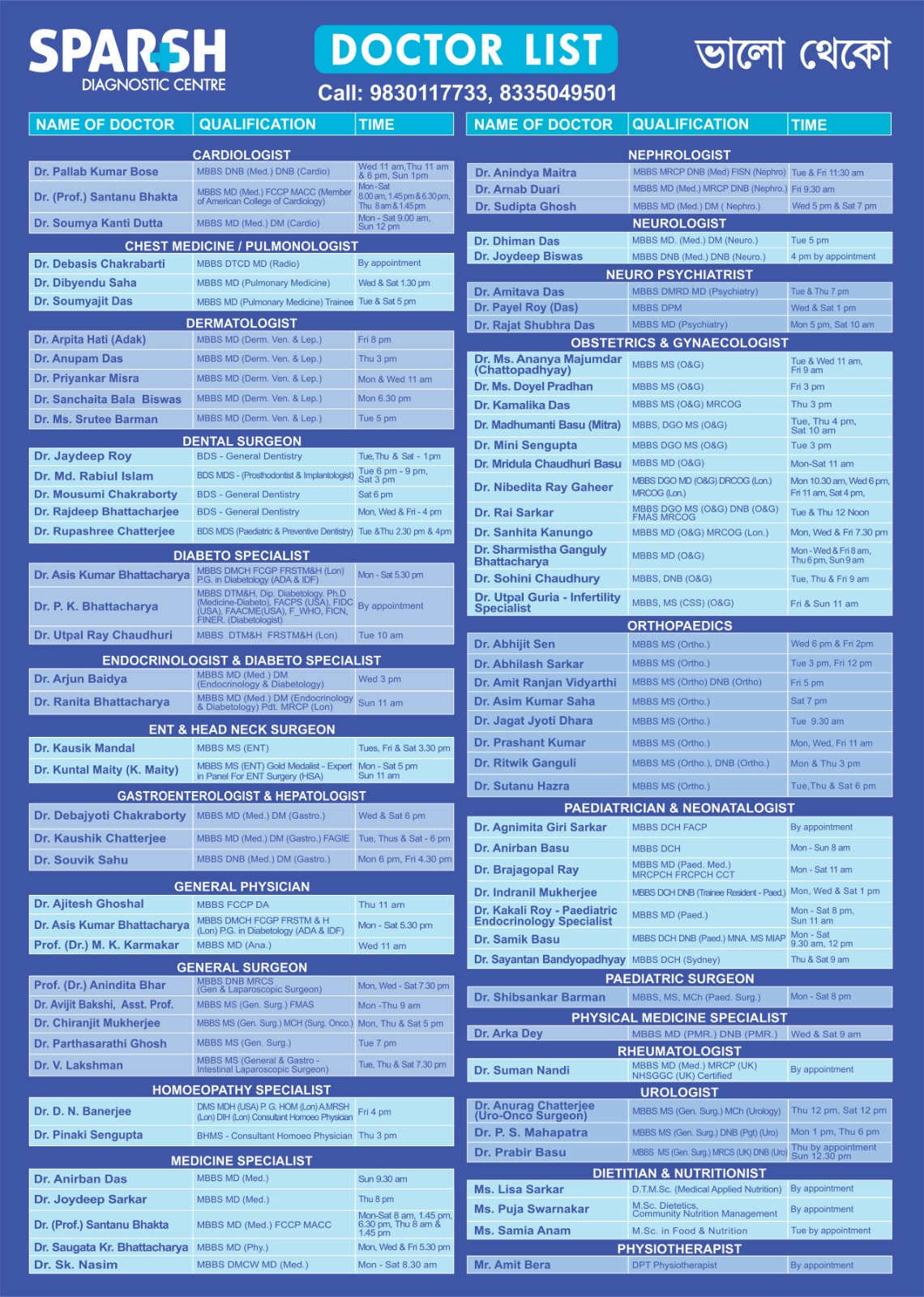
Sparsh Doctor List
![]()